In a historically male-dominated field, women in cancer medicine have been quietly blazing a trail in research and discovery for decades. With less celebrity and recognition, women pioneered advancements, from breakthroughs in experimental research to innovations in cancer treatment and care.
In 1917 with the official admittance of women to Columbia's College of Physicians and Surgeons (P&S), doors were just beginning to open for women who wanted to pursue science and medicine. That fall, 11 women joined a class of 213. Six of the 11 female students would graduate in 1921 holding the first, third, and fifth places in the class.
"One of the difficult things about being a woman in academia was that there were so few of us." -Rosalind Rosenberg, PhD
Five years prior to that milestone, Columbia established in 1912 the Crocker Special Research Fund, its formal program dedicated to the scientific study of cancer and pursuit of a cure. Although the Crocker Fund got its start with half a dozen male faculty members, women soon joined their ranks.
"Women entered medicine at Columbia, and the sciences more broadly, as students, and only much later became faculty members," says historian Rosalind Rosenberg, professor emerita at Barnard College and author of "Changing the Subject: How the Women of Columbia Shaped the Way We Think About Sex and Politics."
New York City's burgeoning female workforce
Around the time that cancer research started to blossom at Columbia and P&S went offiicially coed, New York City also was seeing an influx of women moving to the city and the workplace.
According to Dr. Rosenberg, "New York became the capital of the female worker precisely because it could not satisfy its labor needs with men, whose best opportunities lay in the big industries that New York did not have. New York was the center of America's consumer culture; the country's productive life lay elsewhere … [Women] worked as domestic servants, garment workers, and retail clerks. But the demand for educated women expanded dramatically as the economy grew more complex. Indeed, the more education the women had, the more likely she was to be employed. Nearly half of the women who graduated from Barnard College in 1900 joined the workforce and were still there 15 years later."
Pre- and post-World War II witnessed another flood of women in the workforce, including positions as researchers, technicians, and assistant professors at P&S. By the 1970s, with Columbia's affirmative action program in place, minorities and women academics were recruited and hired to join faculty ranks. By then, more women students, faculty, and staff could be seen gracing the halls and labs at Columbia but the work environment remained difficult for women to advance. Groups or societies dedicated to supporting women and their careers or led by women did not exist as they do now.
"One of the difficult things about being a woman in academia was that there were so few of us," recalls Professor Rosenberg, who was one of the first women to join the faculty at Columbia's history department in 1974, as part of the University's newly established affirmative action program. "It was a pretty lonely time. In those days, women were trying as much as possible to look like the men, in the hope of keeping their jobs."
Meanwhile, women researchers and faculty at P&S had been contributing solutions to the problem of cancer since the beginnings of the cancer program at Columbia. Though many of their achievements were left untold, these early women pioneers helped lay the foundation for discovery and innovation in cancer for decades to come.
Making history in Columbia's early days of cancer research and medicine

Edith H. Quimby, ScD
Professor of radiology at the College of Physicians and Surgeons
Edith H. Quimby, ScD, a pioneering medical physicist, began studying the therapeutic use of X-rays and radium in 1919, when these discoveries were still very new. Her first job was as a temporary assistant physicist in a lab led by Dr. Gioacchino Failla, chief physicist at New York City Memorial Hospital. Drs. Quimby and Failla would become close research collaborators for more than 40 years. In 1942, she joined the College of Physicians and Surgeons (now the Vagelos College of Physicians and Surgeons) as associate professor of radiology, with Dr. Faillia. She was promoted to full professor in 1954.
Dr. Quimby, who led an active radioisotope lab at Columbia until her retirement in 1960, is best remembered for the "Quimby Rules," a system used by radiation oncologists to guide placement of radium needles for cancer treatment. Her work focused on the medical effects of radiation and how to determine the precise dosage needed that would cause the fewest side effects. She co-authored "Physical Foundations of Radiology," the first physics textbook for radiologists.
Dr. Quimby received numerous honors and awards, among them the 1940 Janeway Medal from the American Radium Society. When she was elected president of the American Radium Society in 1954, she was the first woman to do so. The Edith H. Quimby Lifetime Achievement Award of the American Association of Physics in Medicine is named in her honor.
David Brenner, PhD, professor of radiation biophysics at Columbia and director of the Center for Radiological Research, calls Dr. Quimby an "incredible inspiration." He says, "Quimby was one of the very first scientists to show that radiotherapy doses and treatment times could really be used to improve the outcome of cancer radiotherapy, and that concept has always motivated my own research into optimizing radiotherapy treatment protocols."
Ethel B. Gutman, MD
Researcher in Ophthalmology, assistant professor in Medicine at the College of Physicians and Surgeons, and a clinical chemist at Presbyterian Hospital (now NewYork-Presbyterian)
In 1938, Drs. Alexander B. Gutman and Ethel Gutman reported increased levels of acid phosphatase in patients with metastatic prostate cancer. The husband-and-wife team developed the acid phosphatase test, noted as one of the most useful of all blood tests for cancer, specifically to determine prostate cancer. Shortly thereafter, scientists Dr. Charles Huggins and his student, Clarence Hodges, of University of Chicago discovered that men with prostate cancer treated by surgery (removal of one or both testicles) or estrogen injections experienced regression of their disease, correlated with a significant decrease in their acid phosphatase levels. These findings formed the foundation of androgen deprivation strategies. The findings also established acid phosphatase as a tumor marker for prostate cancer. Though the Gutmans are listed on scientific papers jointly for their discovery of the acid phosphatase test, there has been little promotion of Ethel's involvement in the finding or her additional achievements.
Alexander joined P&S in 1929 and served until 1967, rising from assistant to a full professor of medicine. In addition to his work with Ethel on prostate cancer, Alexander was also credited with developing a major new treatment for gout. According to an appointment card at Columbia Archives & Special Collections, Ethel worked as a researcher in Ophthalmology and an assistant professor in Medicine at P&S, beginning in 1921. The appointment card noted the date of her death as March 6, 1946.

Maynie Rose Curtis, PhD
Associate in cancer research at the Crocker Special Research Fund (ancestor to the Herbert Irving Comprehensive Cancer Center)
Wilhelmina F. Dunning, MD
Associate in cancer research at the Crocker Special Research Fund
Drs. Maynie Rose Curtis and Wilhelmina F. Dunning were close collaborators on the development of animal models to study cancer. At the time, the 1920s, this remained a challenge in cancer research and there was a pressing need for a reproducible animal model to study the disease. Dr. Curtis joined the Crocker Special Research Fund just five years after its launch in 1917. Prior to teaming up with Dr. Dunning, she worked closely for years with pathologist Frederick D. Bullock, PhD, at the Crocker Fund, reporting their first success in 1920 in producing sarcomas in animal models, namely rats.
Dr. Dunning MD'28 first joined Drs. Curtis and Bullock as a student and then fulltime as a researcher in 1932. Dr. Dunning analyzed the data generated from studies conducted with the sarcoma models. Between 1933 and 1940, numerous studies were conducted using the inbred rat colonies produced at Columbia by the trio. The "Dunning rat", used by researchers to investigate prostate cancer and tumor biology, was developed by Dr. Dunning. In a 1978 retrospective summary of events, Dr. Dunning wrote, "A 'rat village' of some 10,000 individuals was built up, composing of as many divergent strains as was practicable and with the greatest attainable biological uniformity within each line. This colony has been under observation for more than 20 years."
Both Drs. Curtis and Dunning retired from Columbia in 1941 when the cancer research program was relocated to the medical school and renamed the Institute of Cancer Research.
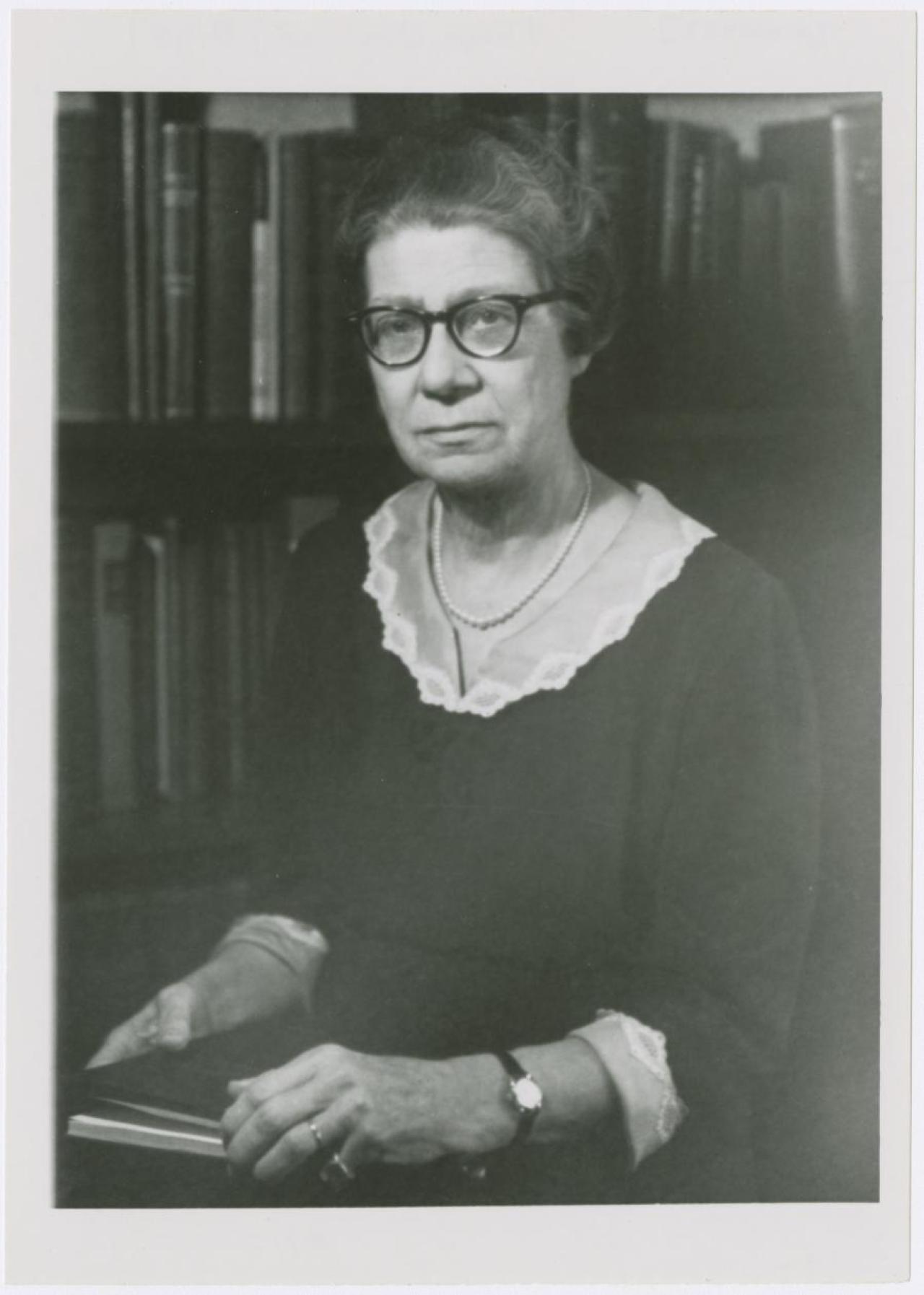
Virginia Kneeland Frantz, MD
Surgical pathologist at Columbia and NewYork-Presbyterian and 1922 graduate of the College of Physicians and Surgeons
As one of the early pioneers of surgical pathology, Dr. Virginia Kneeland Frantz made a series of important cancer discoveries. In the 1940s, she was among the first to demonstrate that radioactive iodine was effective in diagnosing and treating metastatic thyroid cancer. With surgeon Dr. Allen O. Whipple, she was the first to describe the insulin-secretion of pancreatic tumors, and her text on tumors of the pancreas-the Armed Forces Atlas of Tumor Pathology-became the standard on the subject.
Her medical contributions also extended outside the field of cancer. During World War II, Dr. Frantz studied the control of bleeding during surgery and helped discover how oxidized cellulose could aid wound healing. The product was developed under her direction and used on the battlefield. For her military contributions, Dr. Frantz received the Army-Navy Certificate of Appreciation for Civilian Service.
Dr. Frantz was the first woman to pursue an internship in surgery at Presbyterian Hospital (now NewYork-Presbyterian) and the first woman to become president of a major national medical organization, the American Thyroid Society. Columbia University Irving Medical Center established the Virginia Kneeland Frantz Society in 2014 to serve, support, and celebrate the careers of women in science and medicine at Columbia.
Anneliese Sitarz, MD
Professor of Pediatrics at the College of Physicians and Surgeons and 1954 graduate of P&S
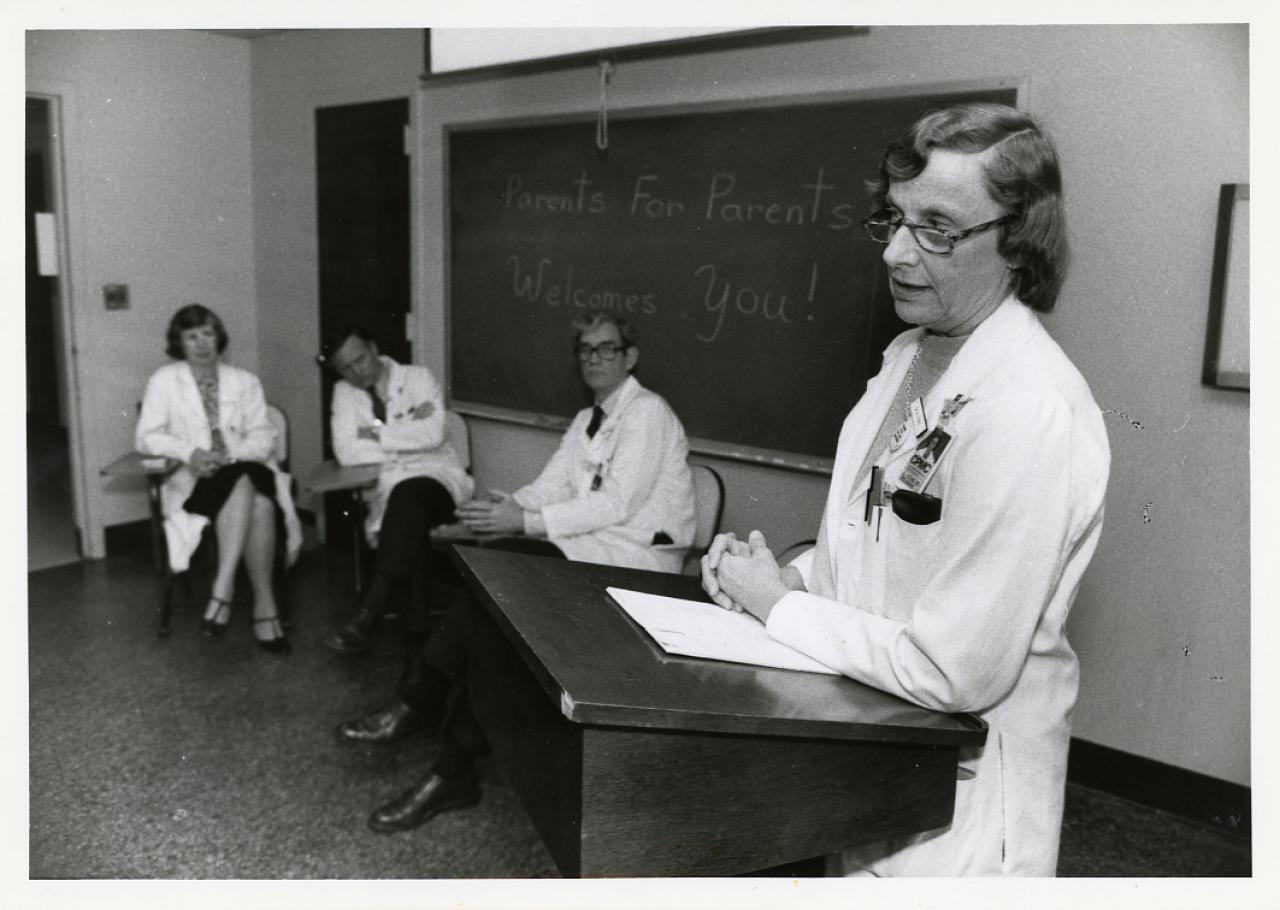
When Dr. Anneliese Sitarz began her more than five-decade career in pediatric hematology and cancer care in 1954, less than 10 percent of children with cancer were cured. Now nearly 80 percent will survive a cancer diagnosis. Dr. Sitarz trained at Babies Hospital, the predecessor to Morgan Stanley's Children's Hospital at NewYork-Presbyterian, and later joined the staff and rose to the rank of professor in 1983 at Columbia P&S.
In 1955, pediatric cancer research got a jolt of funding when the National Cancer Institute established the Children's Cancer Group, aimed at developing new treatments for pediatric cancer. At Columbia, Dr. Sitarz became a founding investigator of that initiative, leading trials, primarily at Babies Hospital, to study novel therapies for pediatric leukemia as part of the Children's Cancer Study Group (CCSG). Her landmark paper in 1965 documented that pediatric patients with a variety of solid tumors could benefit from chemotherapy that had been used to treat leukemia. Dr. Sitarz also served on the NCI committee which established the criteria for evaluating children's response to therapy. Among many accomplishments, Dr. Sitarz computerized a pediatric tumor registry from 1948 to the mid-1980s, the oldest in the U.S.
In addition to her research in pediatric oncology and new treatments, Dr. Sitarz was well-regarded for her compassionate care and placing an emphasis on the importance of supporting families and caregivers of the children suffering from cancer as much as the patients themselves. She ran a community program at Babies Hospital called "Parents Caring for Children with Cancer" that routinely brought together pediatric oncologists and psychologists to answer questions and provide guidance to families and caregivers.
At a retirement dinner held at P&S in her honor in 2008, she said, "I can think of nothing more rewarding than to have been able to play a decisive role in increasing the survival of the many children with these terrible diseases."






