Leiden chemists recreated the bacterial capsule of meningococcus in the lab. With a few modifications, these capsules can serve as an extra safe and effective vaccine against these notorious bacteria, which can cause, for example, meningitis. PhD candidate Jacopo Enotarpi and his team published the first promising results in Nature Communications.
Meningococcus
'Our group investigates how the immune system reacts to various bacterial structures,' says Enotarpi. We recreate these structures in our lab. This knowledge is essential for the development of new vaccines against bacteria. This is important, especially now that bacteria are becoming increasingly resistant to the antibiotics that have been able to protect us so far'.
The researchers focused on the meningococcal bacterium, which causes serious infections such as meningitis. 'The type of meningococcus we looked at is responsible for epidemic meningococcal outbreaks in African developing countries,' says Enotarpi. The recent introduction of a vaccine has dramatically decreased the disease incidence. 'However, this vaccine is not yet stable enough to be commercialised in a fully liquid form.'
How does it work?
With vaccination, you bring an attenuated or dead pathogen into the body. The body can easily overcome this weak pathogen and will also memorise how to do so. This way, if the next infection (of a healthy bacterium or virus) occurs, your weapons are all set: you can quickly defuse the pathogen and don't get sick.
Sugar coats
The meningococcal vaccine mentioned above is different from traditional vaccines, which usually consist of live attenuated bacteria or dead whole-cell bacteria. It is a so-called subunit vaccine that contains only a small purified component of the pathogen. The meningococcal vaccine contains so-called bacterial capsules. These are sugar coats that protect bacteria from intruders. But the capsules also have a drawback for the bacteria: the host's immune cells can recognise the bacteria by the capsule and thus attack more easily. For this reason, bacterial capsules are a great ingredient for a vaccine.
However, there is one problem with capsule vaccines: the capsules do not activate the memory of the immune system. The immune system defeats the capsules without remembering how to do so. This means that the body is not protected against a subsequent infection (see box). Luckily, this problem can be solved by adding a special transport protein, which does activate the immune memory.
Synthetic structures
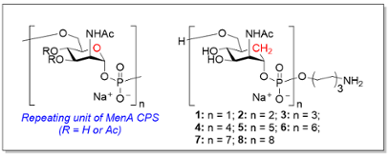
In order to further increase the safety and efficiency of subunit vaccines, Enotarpi and his team have now recreated the bacterial capsules in the lab. 'If you make large batches of vaccine based on live-attenuated or whole-cell killed bacteria, the composition will be heterogeneous. Bacteria deactivation and purification is a difficult process and the end result is not always a hundred per cent the same. This means the composition of each individual shot is just a little different. Vaccine batches based on synthetic capsules are homogenous and therefore induce a more robust and consistent response.'
Enotarpi: 'Our synthetic fragments do not only resemble the natural structure but also contain a small chemical modification which increases the stability of these structures in water. This small modification can only be made by synthesis.' The team conjugated the particles to a transport protein to test whether they could actually generate a long-lasting reaction from the immune system in mouse models. And with success: 'We saw that after vaccination with our synthetic capsules there were as many antibodies in the body as after vaccination with the vaccine based on natural structures. The vaccine we made actually represents the first capsule mimetic vaccine that is really active. I hope our research is a helpful contribution to the fight against antibiotic resistance.'
Further reading:
C2W.nl: Suikerlaagmimetica als vaccinbasis (in Dutch)






