New work by a University of Illinois Urbana-Champaign scholar harnesses the power of generative artificial intelligence, using it in tandem with measurement-based care and access-to-care models in a simulated case study, creating a novel framework that promotes personalized mental health treatment, addresses common access barriers and improves outcomes for diverse individuals.
Social work professor Cortney VanHook led the research, in which he and his co-authors used generative AI to simulate the mental health journey of a fictitious client named "Marcus Johnson," a composite of a young, middle-class Black man with depressive symptoms who is navigating the health care system in Atlanta, Georgia.
In response to the researcher's prompts, the AI platform created a detailed case study and treatment plan for the fictional client. Based on the personal details that the researchers used in the prompt, the AI platform examined the simulated client's protective factors such as his supportive family members and his potential barriers to care ― including gendered cultural and familial expectations ― along with his concerns about obtaining culturally sensitive treatment due to the shortage of Black male providers in his employer-sponsored health plan's network.
Real-world simulations enable practitioners to understand individuals' pathways to mental health care, common access issues and demographic disparities, VanHook said.
Moreover, using a simulated client mitigates concerns about breeching patient privacy laws, thereby enabling practitioners, trainees and students to explore and refine potential interventions in a low-risk environment, promoting more equitable, responsive and effective mental health systems, he said.
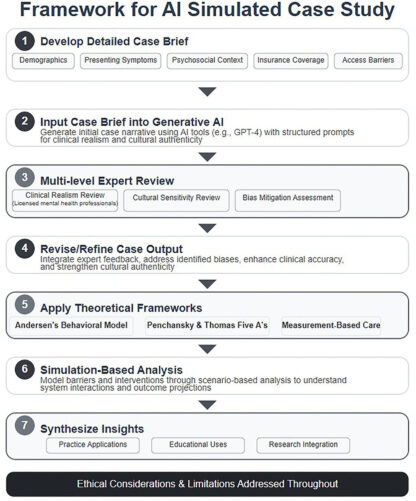
Graphic by Cortney VanHook and Daniel Abusuampeh
"What's unique about this work is it's practical and it's evidence-based," VanHook said. "It goes from just theorizing to actually using AI in mental health care. I see this framework applying to educating students about populations they might not be familiar with but will come in contact with in the field, as well as its being used by supervisors in the field when they're training their students or by clinicians on how to understand and best support clients that come to their facilities."
VanHook and co-authors Daniel Abusuampeh of the University of Pittsburgh and Jordan Pollard of the University of Cincinnati prompted the AI platform to apply three theoretical, evidence-based frameworks in creating its simulated case study and treatment plan for the virtual client.
The AI software was prompted to use Andersen's Behavioral Model ― a theory about the factors that determine individuals' health services utilization ― to examine the personal, culture and systemic factors that supported or hindered the client's use of mental health services. In addition, the proposed treatment plans incorporated a theory about the five components of access to evaluate the availability, accessibility, accommodation, affordability and acceptability of care for the client; along with Measurement Based Care, a clinical approach that applies standardized, reliable measures for ongoing monitoring of the client's symptoms and functioning.
The team used measurement-based care to refine the treatment approaches recommended by AI. To ensure that the AI-generated simulation reflected real-world clinical practice, VanHook and Pollard ― who are both licensed mental health professionals ― reviewed the proposed treatment plan to verify its clinical accuracy and compared the case brief against published research findings.
As all three authors identify as Black men, they confirmed the materials' cultural sensitivity and conceptualization of the barriers that Black men often face in the U.S. mental health system.
"Every population ― regardless of race, age, gender, nationality and ethnicity ― has a unique mental health care pathway, and there is a lot of information out there in AI to understand different populations and how they interact with the mental health field. AI has the ability to account for the complex barriers as well as the facilitators of population-wide mental health care," VanHook said.
The authors acknowledged that the content generated by AI technology will be limited by the data and patterns in the platform's training set, which may not reflect the diversity, unpredictability or emotional nuances of clinical encounters. Likewise, despite the evidence-based frameworks that were applied in the project, VanHook said these do not address all of the systemic and structural barriers experienced by Black men or capture every social, cultural or individual factor that influences clients' care.
Nonetheless, the team maintained in the paper, which was published in the journal Frontiers in Health Services, that generative AI holds significant promise for improving access, cultural competence and client outcomes in mental health care when integrated with evidence-based models.
"AI is a train that's already in motion, and it's picking up speed. So, the question is: How can we use this amazing tool to improve mental health care for many populations? My hope is that it is used in the field, as a tool for teaching and within higher order management and administration when it comes to mental health services," VanHook said.
In August, Illinois Gov. JB Pritzker signed a new law ― The Wellness and Oversight for Psychological Resources Act ― that limits the use of AI in mental health care "to administrative and supplementary support services" by licensed behavioral health professionals. The new policy came in response to reports of youths in the U.S. committing suicide after interactions with AI chatbots.
"The use of AI in the manner in our study complies with the new state law if it is used in the process of education and clinical supervision," VanHook said. "The measurement-based process described may blur the lines, so I would urge caution against its use beyond education and clinical supervision purposes until we receive more guidance from the state."






