June Y. Hou, MD
Regular cervical cancer screening using HPV testing and/or Pap tests can prevent up to 90% or more of cervical cancers by detecting and treating precancerous lesions early, making it one of the most preventable cancers. Yet, only about 75% of women are screened as recommended. Barriers such as lack of health insurance, limited access to care, and pain or discomfort associated with Pap tests continue to prevent many people from getting screened. New federal guidance issued this month expands screening options for cervical cancer with a self-collection method that can now be done at home.
June Y. Hou, MD, associate professor of obstetrics and gynecology and the interim Director of Gynecologic Oncology at Columbia University Irving Medical Center/NewYork-Presbyterian, focuses her research on equitable healthcare and innovative screening methods. In this Q&A, Dr. Hou explains what the new guidelines mean, how self-collection works, and who has the new option for at-home testing.
Can you walk us through the timeline of recent updates to cervical cancer screening using HPV testing?
Cervical cancer screening has undergone a series of important updates in the past year, reflecting a growing emphasis on access- and care that puts patients first. In January 2025, the U.S. Preventive Services Task Force (USPSTF) issued updated guidelines recommending self-collected HPV testing as an option for cervical cancer screening, with the goal of reaching more women who face barriers to traditional in-office care.
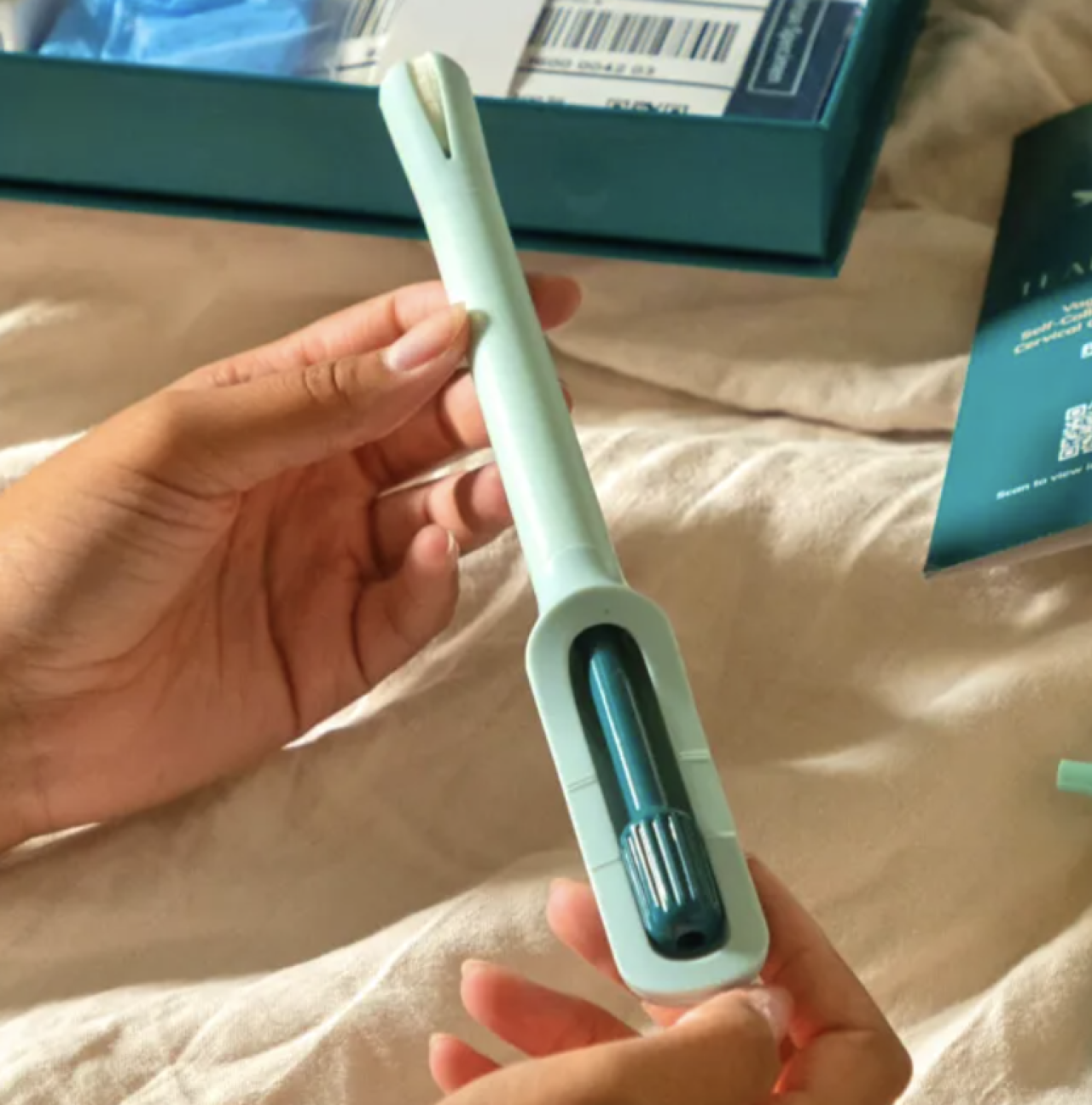
First FDA approved at-home self-collection cervical cancer screening kit, the Teal Wand. Photo credit: Teal Health
Initially, self-collected HPV tests were approved only for use in healthcare settings, such as clinics or doctors' offices. A major milestone followed in May 2025, when the FDA approved the first at-home self-collection cervical cancer screening kit, the Teal Wand, allowing women to screen in their own homes rather than requiring an in-person visit at a healthcare setting.
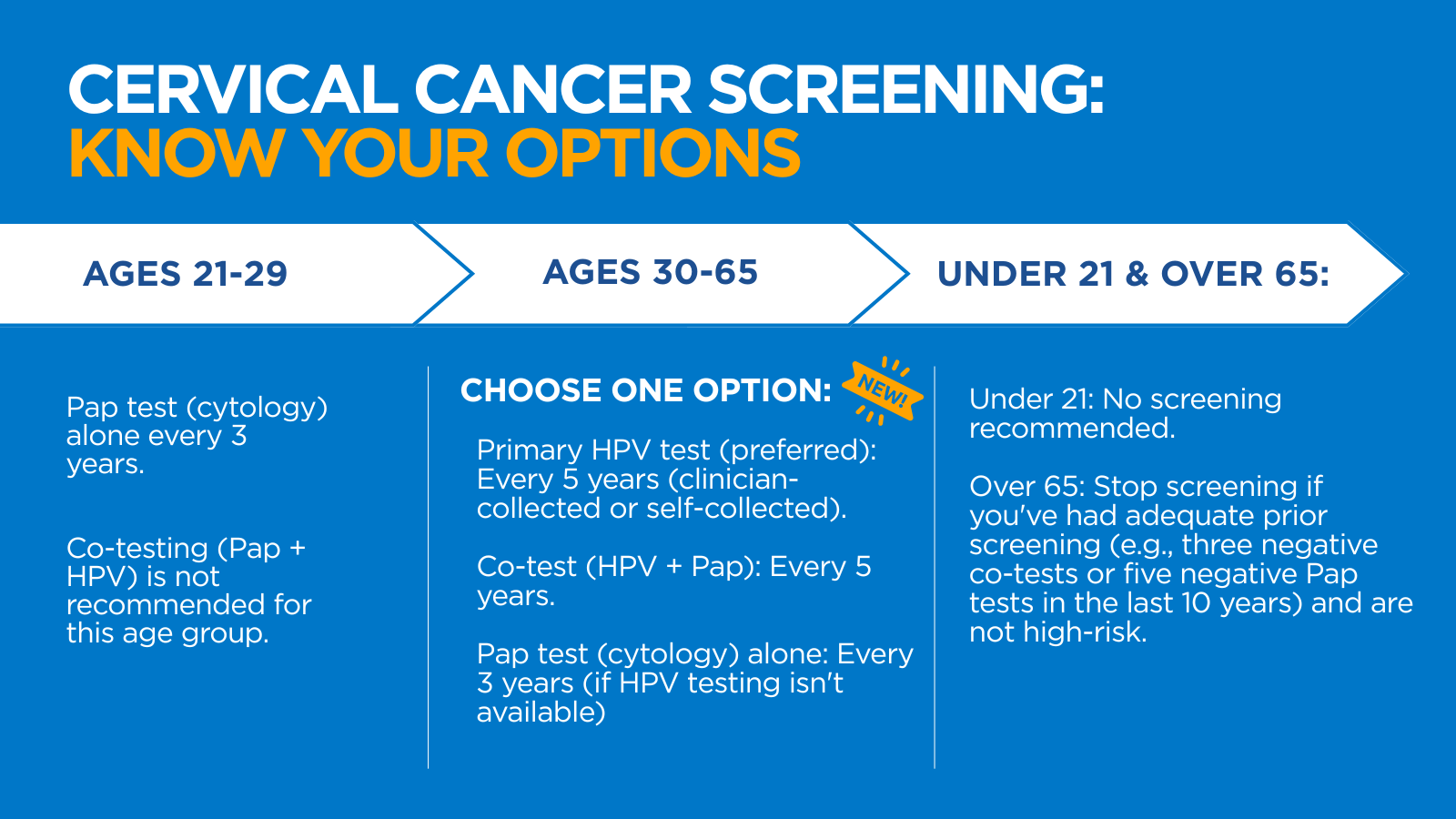
Now, in the most recent round of cervical cancer screening updates, the Health Resources and Services Administration (HRSA) updated its guidelines to include an at-home self-collection option for high-risk HPV (hrHPV) testing. Under these updated recommendations, HPV testing is now the preferred screening method for average-risk women ages 30 to 65.
Importantly, most private insurance plans will be required to cover this new screening option, including any necessary follow-up testing, beginning January 1, 2027.
Traditional screening approaches are still available, including co-testing (HPV and Pap test) every five years, or a Pap test alone every three years. These options help make sure women and healthcare providers can choose the option that best fits their needs and lifestyle.
How does the HPV at-home test work?
For now, most patients access the at-home HPV screening test by completing a questionnaire, and a telehealth virtual visit with one of Teal Health providers. Once eligibility is confirmed, the test will be ordered by the provider and mailed home- with clear instructions on how to collect a vaginal sample yourself and mail it back to the laboratory for testing.
All results are available and accessible to the patient and reviewed by the Teal Health provider. If their results warrant a follow up, it will be coordinated with an OB/GYN. Patients also have the option of sharing their results with their primary OB/GYN and providers of choice.
If results are negative for high-risk HPV, screening with self-collection should be repeated every three years.
Are Pap tests still recommended for women ages 21-29?
Yes. In people ages 21 to 29, HPV infection is very common and often short-lived. The immune system typically clears the virus on its own, and most infections in this age group do not lead to cancer. HPV testing in younger individuals could result in unnecessary follow-up procedures. For this reason, Pap testing alone every three years remains the recommended screening method for this age group.
How are HPV testing and Pap tests different?
Almost all cervical cancers are caused by the human papillomavirus (HPV) infection. Cervical cancer screening aims to detect precancerous changes in the cervix before they develop into cancer. A Pap test, which has been the primary method for cervical cancer screening for years, involves collecting cells directly from the surface of the cervix during a pelvic exam using a speculum and a cytobrush. A pathologist then examines the cells under a microscope to look for abnormalities. This 'cervical cytology' identifies cells that have already become precancerous, often from HPV.
The HPV test, which until now was only done in concert with the Pap test, detects high-risk HPV DNA from cells collected from the cervix and/or vagina. It is an extremely sensitive method for detecting high-risk HPV, which is the major risk factor for precancer and cancerous changes of the cervix. HPV testing detects more high-grade precancerous lesions than Pap testing alone.
The new guidelines come in the wake of recent research demonstrating the effectiveness of at-home HPV testing compared to testing administered by a clinician. The major difference for patients is that they will no longer have to go to the doctor for the test or require a pelvic exam.
Could at-home self-collection help improve screening rates?
Yes. This option is especially important for people in medically underserved areas, those without insurance, and those for whom a pelvic exam is not feasible or acceptable.
Research shows that many under-screened individuals already visit healthcare providers for other medical needs but may not seek gynecologic care. The flexibility of at-home testing means screenings can be integrated into routine life for women more easily, helping detect potential problems earlier and improve cervical cancer outcomes.
Countries that have already adopted the self-collected tests have already seen improved screening rates, and some experts suggest that with continued adoption, cervical cancer could even be completely eliminated.






