DiaCardia, a novel artificial intelligence model that can accurately identify individuals with prediabetes using either 12-lead or single-lead electrocardiogram (ECG) data, has been recently developed. This breakthrough holds promise for future home-based prediabetes screening using consumer wearable devices, without requiring invasive blood tests. This study emphasizes the utility of the ECG as a powerful biomarker and highlights that the innovative AI model can contribute to the prevention of diabetes.
Towards AI-Based Prediabetes Detection Using Electrocardiogram (ECG) Data
Type 2 diabetes occurs when the human body either cannot make enough insulin or does not use insulin well, resulting in high blood glucose levels. This condition is a growing global health burden that can reduce the quality of life and life expectancy. Before type 2 diabetes develops, many people go through a prolonged stage called prediabetes, where blood glucose levels are above normal but not high enough to be diagnosed as diabetes. Prediabetes is an important window wherein lifestyle changes can reduce the progression to diabetes.
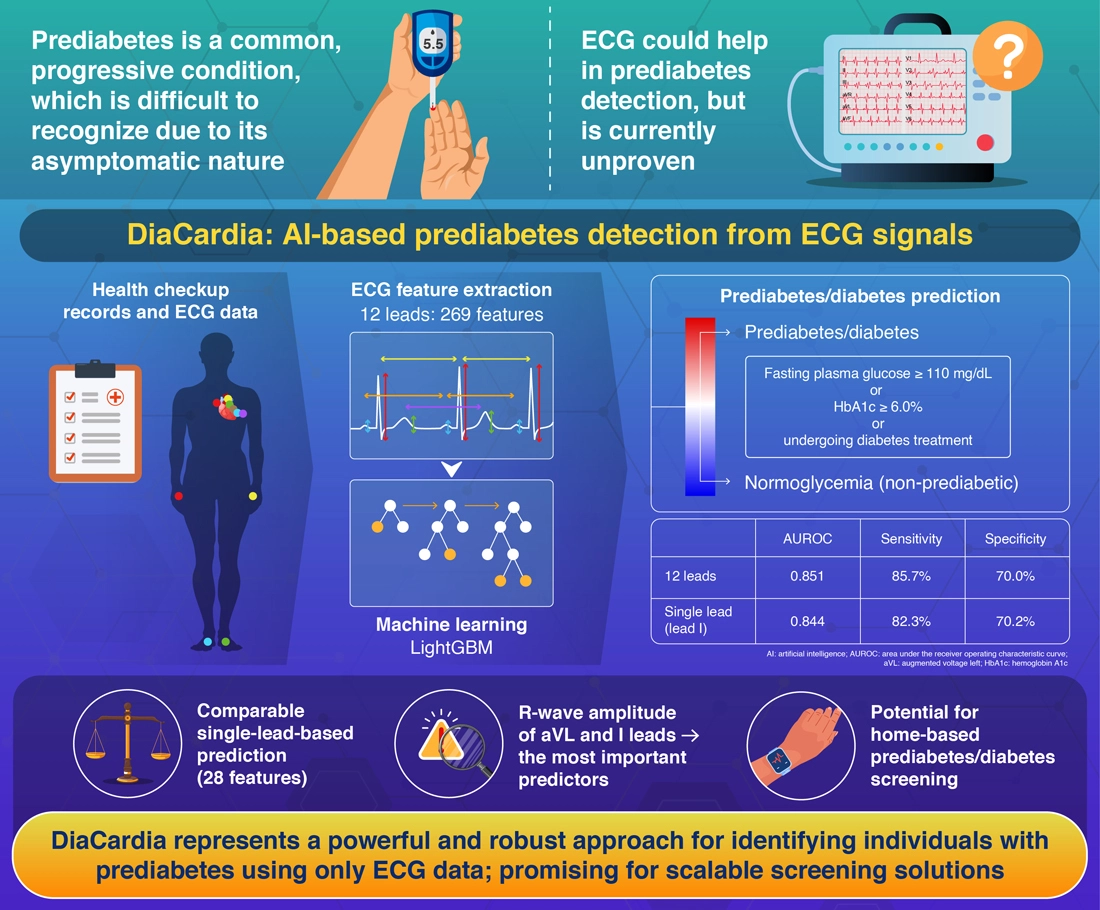
Unfortunately, early detection of prediabetes is challenging due to its asymptomatic nature, low participation in health checkups, and the costs of blood tests. An electrocardiogram (ECG) is a standard test for monitoring cardiac electrical activity. Since prediabetes is also known to increase the risk of cardiac diseases, ECG measurements could be used to screen for prediabetes. Recent studies using deep learning models have combined ECG data with other patient information, such as age and sex, to detect 'diabetes.' However, accurate detection of 'prediabetes' using ECG data alone has not been demonstrated.
In a new study, a research team led by Junior Associate Professor Chikara Komiya, graduate student Dr. Ryo Kaneda, and Professor Tetsuya Yamada from the Department of Molecular Endocrinology and Metabolism, Institute of Science Tokyo (Science Tokyo), Japan, developed a new artificial intelligence (AI) model called DiaCardia that can identify individuals with prediabetes using only ECG readings. The team also included Researcher Daisuke Koga (currently, Assistant Professor at Saga University), Junior Associate Professor Satoshi Ohno and Professor Hideyuki Shimizu from the Department of AI Systems Medicine, M&D Data Science Center, Institute of Integrated Research, Science Tokyo, and Professor Hideki Katagiri from the Department of Diabetes, Metabolism and Endocrinology, Tohoku University Graduate School of Medicine, Japan. Their study was published in Volume 24 of the journal Cardiovascular Diabetology on November 11, 2025.
"This is the first robust, interpretable, and generalizable AI model capable of identifying individuals with prediabetes using either 12-lead or single-lead ECG data," explains Komiya.
DiaCardia is based on the LightGBM machine learning algorithm, which the team selected after comparing multiple models. For training and testing, the researchers utilized 16,766 health checkup records from a single clinic in Tokyo, where each record consisted of multiple health metrics, including fasting plasma glucose (FPG), hemoglobin (Hb) A1c levels, and standard 12-lead ECG data. The dataset was divided into separate training and internal testing groups.
Prediabetes/diabetes was defined to meet at least one of the three criteria: FPG ≥110 mg/dL, HbA1c ≥6.0%, or undergoing diabetes treatment. The model utilizes 269 waveform features extracted from 12-lead ECG signals.
In internal testing, the model identified individuals with prediabetes with impressive accuracy, achieving an area under the receiver operating characteristic curve (AUROC) of 0.851, using ECG data alone. It also exhibited robust performance in an external validation dataset from another institution without any retraining, showing high generalizability. Shapley additive explanations (SHAP) analysis identified higher R-wave amplitudes in augmented voltage left and other ECG leads and reduced heart rate variability as the main predictors of prediabetes/diabetes. These features are known to be associated with increased left ventricular mass due to insulin resistance and autonomic neuropathy, respectively, supporting the physiological plausibility of DiaCardia's predictions.
The researchers also conducted an additional analysis in which participants were matched to account for six major confounding factors. DiaCardia still showed substantial predictive power, indicating that the model captures ECG features specific to impaired blood glucose regulation.
Importantly, even when using single-lead (lead I) ECG data with only 28 features, the model demonstrated comparable performance, nearly matching the performance obtained using 12-lead data. This is a key breakthrough that could open new possibilities for home-based prediabetes screening using wrist-worn wearable devices.
"DiaCardia has the potential to make prediabetes screening scalable, accessible, and available anytime, anywhere, without a blood test," concludes Komiya. "By promoting widespread screening of prediabetes, this work will ultimately contribute to the prevention of diabetes."
Reference
- Authors:
- Daisuke Koga2, Ryo Kaneda1, Chikara Komiya1,*, Satoshi Ohno2, Akira Takeuchi1, Kazunari Hara1, Masato Horino1, Jun Aoki1, Rei Okazaki1, Ryoko Ishii1, Masanori Murakami1, Kazutaka Tsujimoto1, Kenji Ikeda1, Hideki Katagiri3, Hideyuki Shimizu2*, and Tetsuya Yamada1
*Corresponding authors
- Title:
- Artificial intelligence identifies individuals with prediabetes using single-lead electrocardiograms
- Journal:
- Cardiovascular Diabetology
- Affiliations:
- 1Department of Molecular Endocrinology and Metabolism, Graduate School of Medical and Dental Sciences, Institute of Science Tokyo, Japan
2Department of AI Systems Medicine, M&D Data Science Center, Institute of Integrated Research, Institute of Science Tokyo, Japan
3Department of Diabetes, Metabolism and Endocrinology, Tohoku University Graduate School of Medicine, Japan






