A Cornell-led study has revealed how a deadly form of pancreatic cancer enters the bloodstream, solving a long-standing mystery of how the disease spreads and identifying a promising target for therapy.
Pancreatic ductal adenocarcinoma is among the most lethal cancers, with fewer than 10% of patients surviving five years after diagnosis. Its microenvironment is a dense, fibrotic tissue that acts like armor around the tumor. This barrier makes drug delivery difficult and should, in theory, prevent the tumor from spreading. Yet the cancer metastasizes with striking efficiency - a paradox that has puzzled scientists.
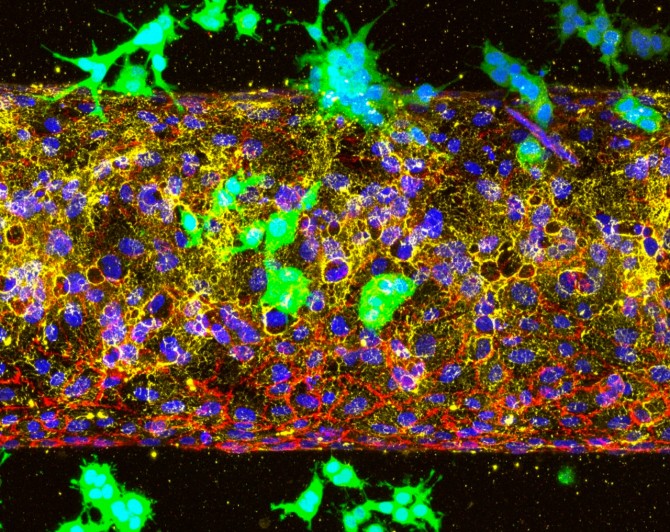
A 3D tumor vessel-on-a-chip model, showing pancreatic cancer cells (green) invading an engineered blood vessel (red) by breaking down the vascular basement membrane (yellow).
New research published in the journal Molecular Cancer reveals that a biological receptor called ALK7 is responsible, by activating two interconnected pathways that work in tandem. One makes cancer cells more mobile through a process called epithelial-mesenchymal transition, and the other produces enzymes that physically break down the blood vessel walls.
"In other words, ALK7 gives pancreatic cancer cells both the engine to move and the tools to invade," said Esak Lee, lead author of the study and assistant professor in the Meinig School of Biomedical Engineering in Cornell Engineering.
The research helps resolve conflicting findings about ALK7, which some studies had linked to blocking cancer spread while others had tied to driving it. Using mouse models of pancreatic cancer and advanced organ-on-chip systems that mimic human blood vessels, the researchers showed that blocking ALK7 significantly slowed metastasis.
The organ-on-chip system, developed in Lee's lab, simulates the tumor microenvironment and is superior to animal models for studying different stages of the cancer. Using it, the researchers studied whether ALK7 drives the initial invasion of blood vessels or the later stage, when circulating tumor cells exit the bloodstream to form new tumors in organs such as the lungs or liver. What they found was that cancer cells couldn't enter blood vessels when ALK7 was inhibited. But when they mimicked a later stage of cancer by placing the cells inside the vessels, they spread quickly, indicating that the timing for treatment is crucial.
"Once we miss this early opportunity to block ALK7 receptors, the cancer cells can freely circulate in the bloodstream and easily seed into other organs," Lee said. "But if we can inhibit ALK7 at the cancer's earliest and most vulnerable stage, we might see better outcomes for patients."
The study also highlights the potential to apply organ-on-chip platforms to study other types of cancers, or how immune cells infiltrate and exit vessels.
"Some cancers have very different microenvironments so, potentially, ALK7 might show different impacts," Lee said. "I hope this study really opens a new avenue for cancer research."
The research was supported by the National Institutes of Health, the National Science Foundation and the National Research Foundation of Korea.
Syl Kacapyr is associate director of marketing and communications for Cornell Engineering.