The Heart Research Institute (HRI) has launched an international research project investigating new therapeutic strategies for stiff heart failure. This exciting new project is supported by a grant funded by HRI UK donors to advance research into cardiovascular disease.
Assoc Prof John O'Sullivan and the Cardiometabolic Disease Group at HRI are collaborating with Prof Christopher Loughrey at the University of Glasgow, Scotland, UK on this project.
Dr Yen Chin Koay, a postdoctoral scientist with the Cardiometabolic Disease Group, is currently working in Prof Loughrey's lab in Glasgow. She provides an update on this critical work.
What is stiff heart failure and how does it differ from other forms of heart failure?
The traditional understanding of heart failure is that left ventricular contraction is impaired such that the heart's output cannot meet the molecular demands of the body. This type of heart failure is now called heart failure with reduced ejection fraction (HFrEF), which denotes the reduced contractile capacity of the left ventricle.
Heart failure with preserved ejection fraction (HFpEF or diastolic heart failure) is a "stiff" type of heart failure where the heart can contract normally but cannot relax properly, due to stiffening of the left ventricle.
How common is stiff heart failure and what impact does it have?
Heart failure affects over 64 million people worldwide; nearly half of these patients have stiff heart failure. In the UK, over 400,000 people have stiff heart failure. In Australia, an estimated 250,000 people have stiff heart failure and over 60,000 Australians are newly diagnosed with stiff heart failure every year.
What kind of treatments are available for stiff heart failure?
Although there are multiple classes of drugs available for HFrEF, they have all failed to demonstrate therapeutic efficacy in HFpEF in clinical trials. A drug called empagliflozin was the first pharmaceutical to demonstrate therapeutic efficacy in HFpEF in the EMPEROR-PRESERVED trial completed in 2021. This is the only pharmaceutical available for HFpEF. Other than this, weight loss and exercise have shown modest benefits.
What happens in heart muscle damaged by heart failure?
During heart failure, or after a heart attack, the heart muscle uses ketones in a different way to supply energy.
Ketones are the most "thrifty" fuel available to the heart. That is, they can extract more energy from ketones with least cost in oxygen consumed (P/O ratio). In HFpEF, there are commonly metabolic constraints that prevent the heart from using glucose, and switching to ketones as a fuel can deliver more energy without consuming so much oxygen, which is critical in this scenario of reduced oxidative capacity. Ketones also have beneficial effects on inflammation and improving mitochondrial biogenesis.
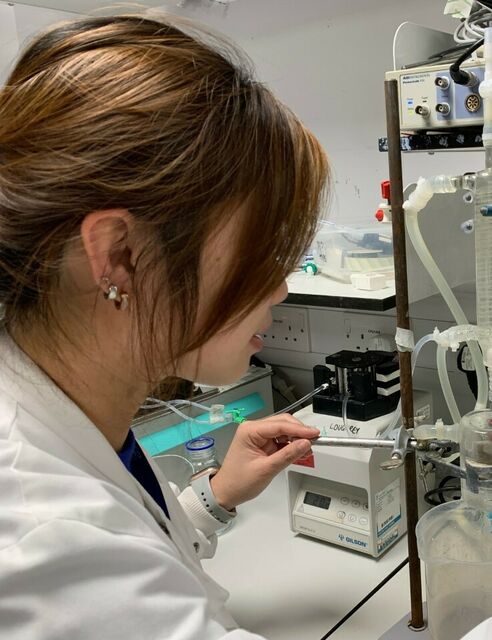
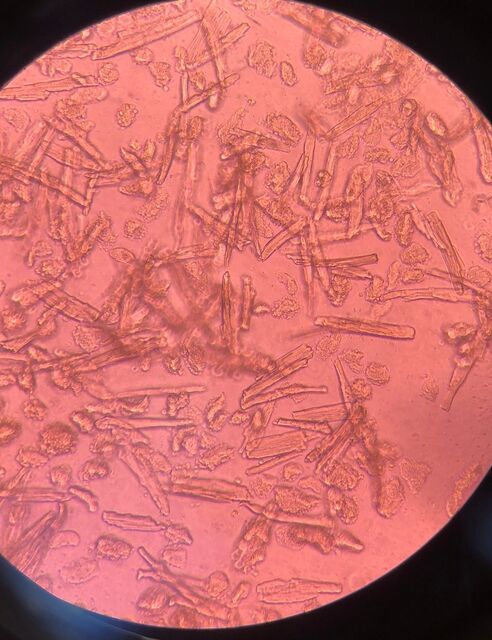

L-R: Dr Yen Chin Koay performing Langendorff isolated heart perfusion; cultured cardiomyocytes from a lab model; The University of Glasgow.
How do you plan to study what happens in heart muscle cells during heart failure?
The heart consumes more energy than all other organs. Most of its energy is produced by the mitochondria inside cardiomyocytes. But these mitochondria need a continuous supply of suitable energy substrates (fuel) to run efficiently. Lack of fuel and incomplete consumption of fuel can lead to the mitochondria being damaged.
For example, if your car engine is given the wrong fuel, it can become damaged, and eventually this will cause problems for the rest of the car. The same is true for the mitochondria inside the heart muscle. Oxidative damage can occur that will ultimately lead to the heart muscle becoming stiffer and developing fibrosis (scarring).
We plan to study the heart's energy needs during HFpEF in collaboration with Prof Roland Stocker, leader of the Arterial Inflammation and Redox Biology Group at HRI. Prof Stocker is an expert in redox biology, which means that he can work with us to measure indicators of oxidative stress in samples taken from stiff heart failure.
How will international collaboration advance this project?
This funding provided by HRI donors will enable the research teams at the University of Glasgow and at HRI in Australia to work in collaboration and learn new techniques from each other. For example, I have come to the University of Glasgow to work with Prof Christopher Loughrey and his British Heart Foundation funded lab team at the College of Medical, Veterinary and Life Sciences (MVLS). I am learning how to isolate cells from the heart muscle and supply them with energy sources so that we can study them for longer. Studying cells in this way means we can do a lot more with the heart muscle samples that we have access to. It's amazing - you can actually see the heart muscle cells beating under the microscope!
The team in Glasgow will also be learning from the research teams at HRI, so there will be a two-way exchange of techniques. What we learn will advance our knowledge of HFpEF and translate our findings to help patients. It will also provide new insights into the role of mitochondria in other conditions, such as myocardial infarction (heart attack).
HFpEF and myocardial infarction are two of the greatest unmet needs in cardiology. Our two groups have complementary skills that are essential to help us understand what causes these conditions and develop new targets for therapy.
What do you hope will be achieved at the end of this two-year project?
Having this collaboration between the research teams at the University of Glasgow and HRI in Australia means that we can exchange techniques and generate high-quality data on HFpEF and myocardial infarction.
We aim to publish the data together in high-impact peer-reviewed journals. We also hope to use what we learn as preliminary data for further research projects. This will help us apply for subsequent funding from the Heart Foundation, NHMRC, NSW Cardiovascular Research Capacity Program, and other funding bodies.
As a researcher coming from Australia, what is it like to work in a lab in the UK?
As a scientist, you should always keep learning. Seeing how a different laboratory does things has really opened my eyes and helped me spread my wings. It also allows me to travel to conferences in Europe that I could not attend from Australia. This all helps me to establish a broader professional network; having a network of colleagues with many different types of expertise means I can prepare stronger grant applications when I return to Australia. It will definitely help my future career.
The grant has also enabled me to share my research on the world stage. In June, I presented my work at an international conference in Berlin, which is held by the International Society for Heart Research (ISHR) every three years. I was awarded the ISHR International Poster Prize - one of 23 prizes awarded by three judges from more than 400 posters!
I really appreciate that HRI has this grant, and I am thankful to Assoc Prof John O'Sullivan, who put me forward for the role, and to Prof Christopher Loughrey and his group for their warm welcome.
To anyone else who has a chance to do this, I would say embrace the change and make the most of the opportunity.
Header image: Freshly isolated cardiomyocytes from a lab sample.






