A naturally occurring protein that tends to be expressed at higher levels in breast cancer cells boosts the effectiveness of some anticancer agents, including doxorubicin, one of the most widely used chemotherapies, and a preclinical drug known as ErSO, researchers report. The protein, FGD3, contributes to the rupture of cancer cells disrupted by these drugs, boosting their effectiveness and enhancing anticancer immunotherapies.
The discovery is described in the Journal of Experimental & Clinical Cancer Research.
The new findings were the happy result of experiments involving ErSO, an experimental drug that killed 95-100% of estrogen-receptor-positive breast cancer cells in a mouse model of the disease. ErSO upregulates a cellular pathway that normally protects cancer cells from stress, said University of Illinois Urbana-Champaign biochemistry professor David Shapiro, who led the new work with Illinois graduate student Junyao Zhu. But when that protective pathway is ramped up, the system goes awry.
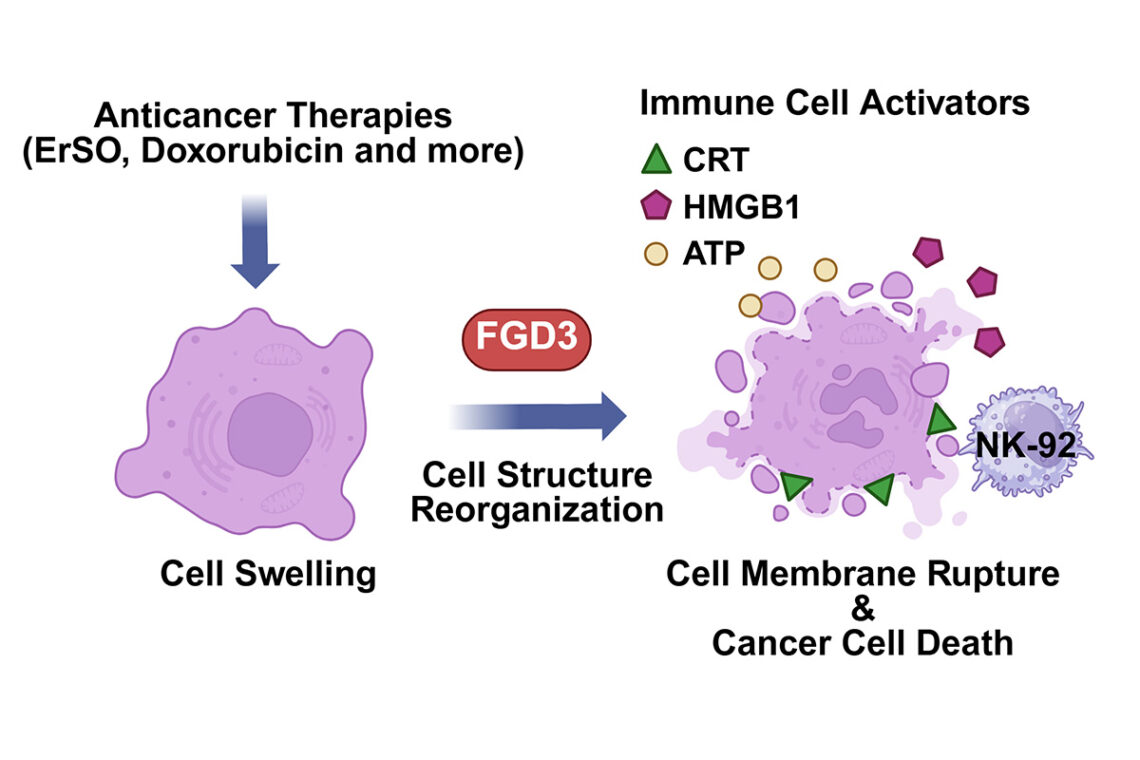
"Most anticancer drugs inhibit something that the cell needs to survive, and they either prevent the cell from growing or, in some cases, cause it to die in an orderly way called apoptosis," Shapiro said. "But ErSO does exactly the opposite. It overactivates the cell pathway and the cancer cells literally swell up and rip open."
Shapiro and U. of I. chemistry professor Paul Hergenrother first discovered ErSO and reported on it in 2021. In the new study, they wanted to better understand how ErSO worked by identifying the cellular proteins that play a role in "making life-death decisions for the cells," Shapiro said.

To do this, they tested the drug against breast cancer cell lines, each of which had one of its 18,000 genes deleted. If a deleted gene undermined the efficacy of a drug - in this case ErSO - it was a signal that that gene played a role in the drug's cancer-killing pathway.
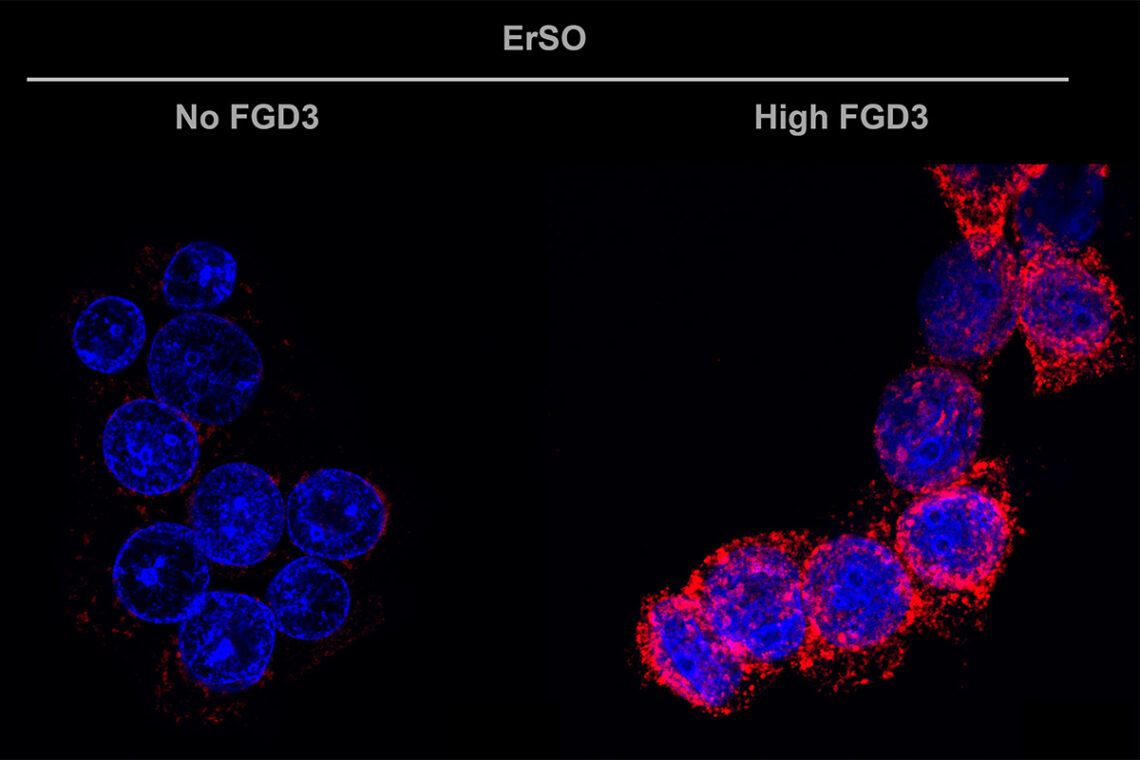
"The top target from the screen with ErSO was the gene for this little-studied protein called FGD3," Shapiro said. "So, we manipulated levels of FGD3 in cancer cells and saw that it indeed controlled whether ErSO could kill the cells. And in a series of important experiments, Zhu showed that FGD3 weakens the cell's architecture."
When not under attack by chemotherapy or other anticancer therapies, FGD3 makes cancer cells more flexible, allowing them to move and change their shape, facilitating their migration and likely increasing their potential to metastasize, the researchers said. But when a drug like ErSO or doxorubicin perturbs the cancer cells, FGD3 causes the swollen cancer cells to rupture.
This rupturing spills out the contents of the cell, alerting the body's immune system, which sends in natural killer cells and macrophages to finish the job, Shapiro said.
The experiments were conducted in 2D cell culture and in 3D "breast cancer patient-derived organoids," which more closely mimic the tumor environment, Shapiro said. Study co-author Dr. Olufunmilayo Olopade, the director of the Center for Clinical Cancer Genetics and Global Health at University of Chicago Medicine, developed the organoids.
"Work from a number of laboratories has shown that these organoids can retain the same pattern of protein production that occurs in the original tumor," Shapiro said.
The team also tested the role of FGD3 in a mouse model of human breast cancer, and they found the same pattern: Higher FGD3 levels enhanced the killing power of ErSO.
"One of the things we saw was that FGD3 dramatically increased the movement to the cancer cell membrane of a protein that stimulates natural killer cells to target a cancer cell for destruction," Shapiro said. "This has the potential for enhancing immunotherapy for cancer and for reducing the doses of toxic drugs that you need to use. This is especially important in breast cancer because immunotherapy has had limited success against solid tumors such as breast cancer."
The research team also analyzed a vast trove of human breast cancer data, looking for patterns between FGD3 levels and responses to various chemotherapy agents.
"We found, with all types of chemotherapy and all classes of breast cancer, there's a very high correlation between the level of FGD3 and whether the patient responds favorably to chemotherapy," Shapiro said. "Those with a high level are highly responsive; those with a low level are poorly responsive. This will allow us to identify those patients most likely to benefit from these kinds of cancer therapies."
"We will try to expand FGD3 into a broader context, to show whether it also plays a role in other cancers and cancer therapies," Zhu said.
"This is a good example of how a scientific study that starts with one objective can broaden out in unexpected directions," Shapiro said. "We started with the question of how our compound worked and then we eventually realized that this is a common pathway shared by a number of anticancer drugs."
Paul Hergenrother is the deputy director, and Shapiro is a member of the Cancer Center at Illinois. Hergenrother also is affiliated with the Carle Illinois College of Medicine and the Carl R. Woese Institute for Genomic Biology at the U. of I.
The National Institutes of Health, the Amend Family Charitable Fund and Systems Oncology supported this research.






