Key takeaways
- Pseudomonas aeruginosa is a species of bacteria that, when organized on a surface to form a community known as a biofilm, causes lethal infections in cystic fibrosis patients and resists treatment with antibiotics.
- A UCLA-led research team has uncovered a key mechanism controlling initial biofilm formation in Pseudomonas, in which cells sense and follow sugar-based trails secreted by other bacteria to organize themselves into a colony on a surface.
- This discovery could lead to treatments for deadly infections in people with cystic fibrosis and in hospitalized patients on ventilators, as well as solutions for problems in industry that are rooted in the presence of bacterial biofilms.
The bacterium known as Pseudomonas aeruginosa is an unwelcome visitor in the human body. Serious infections can result when a bunch of these bugs settle together on a surface to form a biofilm — a community of microbes like the slime on spoiled food, but in this case residing inside a person. The grouped-up bacteria attack the lungs of patients with cystic fibrosis and conditions that require the use of ventilators, such as severe COVID-19. Worse still, the World Health Organization lists Pseudomonas among the antibiotic-resistant bacteria presenting the biggest threat to human health.
Now, however, new findings from researchers led by the California NanoSystems Institute at UCLA (CNSI) reveal just how Pseudomonas go from exploring a surface to committing to it and building a community — a key finding that can help pave the way to understanding how to tackle these types of infections
The new study revealed how Pseudomonas detects and binds to specific sugars left behind by others from its species that arrived earlier. The cell senses these sugar trails using proteins on its body, and then identifies the sugars using hairlike appendages called pili. These pili are normally used to crawl along a surface, but in this case double as mechanical sensors that test the strength of the sugar bonds. All of this information is translated into chemical signals inside the cell that guide the operation of other bacterial machinery, such as the controlled secretion of more sugars to make biofilms.
Reported in the journal Nature Microbiology, the results may inform applications in human health and industry. For Pseudomonas, the findings could lead to better approaches for undermining the dangerous bugs' ability to resist drug treatments.
"We can envision building on these results to influence the bacteria's behavior," said co-first author William Schmidt, a UCLA doctoral student in bioengineering. "We might be able to turn the cells into more antibiotic-susceptible versions of themselves that are easier to treat."
Answers for an enigma of microbiology
Sugar trails secreted by bacteria guide the organization of biofilms. Until now, the mechanisms behind how cells detect sugars secreted by one another on a surface have been unclear. What's more, the cell-membrane proteins that bind to specific sugars lack the necessary structures to allow any signaling, which has been a long-standing puzzle.
The twist revealed by the study is the role of mechanical sensing by pili as the mediator of this signaling.
"This form of signal generation is new to the field," said CNSI member Gerard Wong, a corresponding author of the study and a professor of bioengineering in the UCLA Samueli School of Engineering. "People have thought of pili mostly as appendages for moving around. It turns out they also act as sensors that translate force into chemical signals within bacteria, which they use to identify sugars. We're seeing how sensory information is encoded in bacteria by their appendages for the first time."
The sugars released by bacteria serve as both trails for others to follow and building materials for their communities. At later stages of biofilm development, those bacterial sugars help fix the crowd of bugs in place and form the surrounding matrix of the biofilm that protects from challenges that could dislodge it.
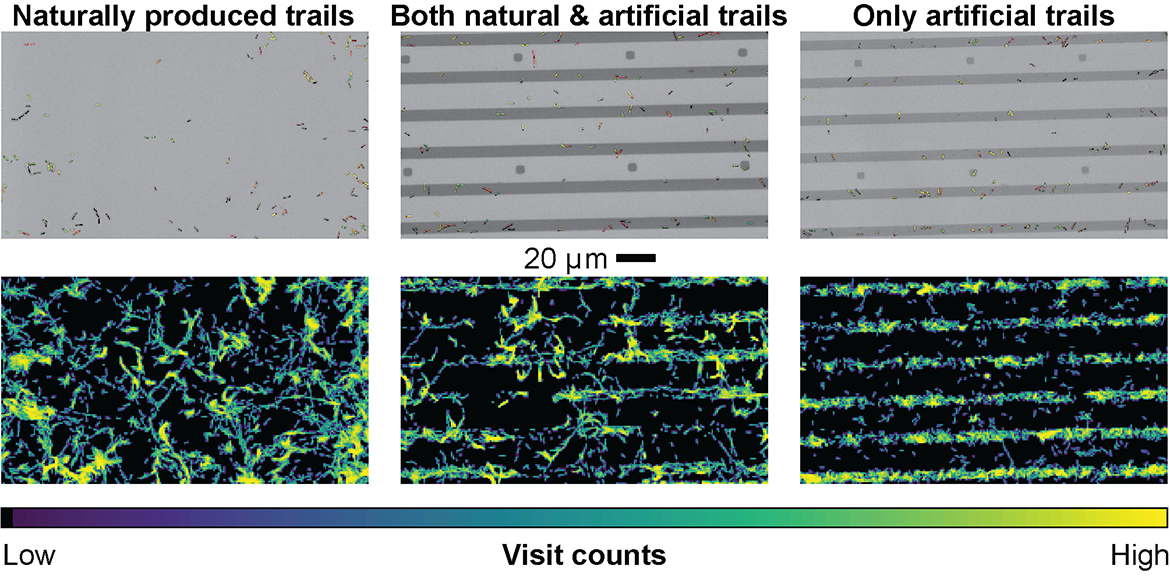
To query this system, the researchers fabricated a surface patterned with premade trails of a synthetic sugar, mimicking the bacteria's naturally produced sugars and especially attractive to Pseudomonas. Using genetic engineering and advanced cell-tracking techniques, the team uncovered the coordinated system combining chemical and mechanical sensing.
What the findings may mean for human health and society
Pseudomonas are much less susceptible to antibiotics when the bacteria are cemented into a biofilm community. They're far more vulnerable while they are in their free-swimming form. Research following up on the CNSI-led study has the potential to yield solutions for Pseudomonas infections in cystic fibrosis patients and others.
"There's the possibility of turning back the clock on biofilm formation," said co-first author Calvin Lee, a UCLA postdoctoral researcher. "Even if you already have a biofilm, you may be able to make the bacteria take it apart by themselves."
The study may also inform solutions to other problems created by bacterial communities. Biofilms foul up pipes and filters as well as reactors used for chemical reactions in industry. They're also the first phase in the accumulations of flora and fauna encrusting ships at sea.
"We can ask, 'Is it possible to make a surface invisible to bacteria?'" said Wong, who is also a professor of chemistry and biochemistry and of microbiology, immunology and molecular genetics at UCLA. "If you get a surface to mimic empty space enough, as far as the bacteria perceive things, it may be possible to solve this multibillion-dollar problem of biofouling."
The researchers are looking into the wider repertoire of sugars sensed by surface proteins in Pseudomonas, as well as how differently shaped surfaces affect the bacteria's travels. The scientists also intend to investigate connections between these findings and previous results indicating that cellular signaling persists across generations of bacteria in biofilms.
George O'Toole of Dartmouth College and Matthew Parsek of the University of Washington are co-corresponding authors of the study. Other co-authors are Jonathan Chen, Kirsten Fetah, James Popoli, Yun Su Choi, Thomas Young, and CNSI members Paul S. Weiss and Andrea Kasko, all of UCLA; and Xuhui Zheng of the University of Washington.
The study received funding from the Army Research Office, the National Science Foundation, the National Institutes of Health, the Cystic Fibrosis Foundation and the Life Sciences Research Foundation. The patterned surfaces used in the study were fabricated at the UCLA NanoLab.






