If Wenjun Zhang has her way, no one will ever have to brush or floss again.
Zhang, a UC Berkeley professor of chemical and biomolecular engineering, is trying to distinguish the healthy bacteria in our mouths from the unhealthy bacteria - those that cause cavities - so that she can boost the proportion of the former and promote a probiotic oral microbiome.
Our mouth's microbiome consists of hundreds of different species of bacteria, many of which form a community that sticks to teeth to form plaque. Previous studies have focused on which of those species are associated with cavities, producing acid that eats away at tooth enamel. But researchers have found that each species is not uniformly good or bad - individual species can have hundreds of different varieties, called strains, that differ in their cavity-promoting qualities.
Instead of focusing on species or strains, Zhang and her team scan the DNA sequences of all the bacteria in the mouth - the metagenome - in search of clusters of genes associated with cavities.
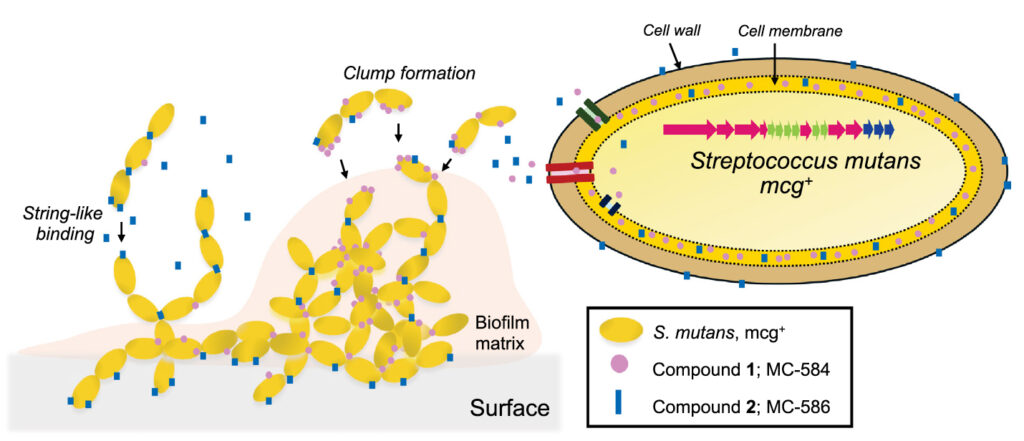
In a paper published Aug. 19 in the journal Proceedings of the National Academy of Sciences, she and her colleagues reported the discovery of one such gene cluster that produces two molecules that together help the mouth's community of bacteria - good and bad - stick together and form a strong biofilm on teeth.
Wenjun Zhang and McKenna Yao/UC Berkeley
They found this gene cluster in some but not all strains of several known bad actors in the mouth, including Streptococcus mutans - the main villain in tooth decay. Zhang sees an opportunity to stick this gene cluster into good bacteria to help them attach better to teeth and push out the acid-producing bacteria that pave the way for cavities.
"Particular strains belonging to the same species can be a pathogen or a commensal or even probiotic," Zhang said. "After we better understand these molecules' activity and how they can promote strong biofilm formation, we can introduce them to the good bacteria so that the good bacteria can now form strong biofilms and outcompete all the bad ones."
The work was supported by the National Institute of Dental & Craniofacial Research of the National Institutes of Health (R01DE032732).
"Specialized" metabolism
The gene cluster was discovered by searching through an online database of a large number of metagenomic sequences of the microbial communities in the mouths of human volunteers. Berkeley graduate student McKenna Yao conducted a statistical analysis to identify clusters associated with oral disease and then cultivated the bacteria to analyze and identify the metabolites produced by these clusters.

Wenjun Zhang and McKenna Yao/UC Berkeley
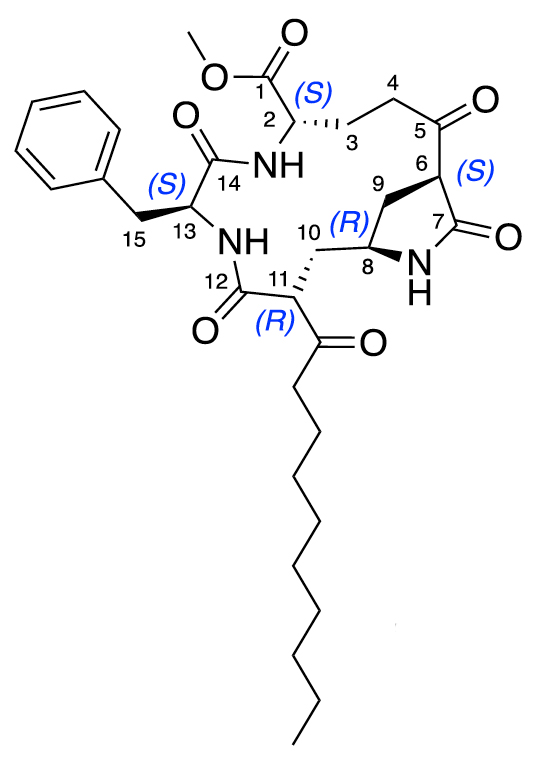
The metabolites are small molecules composed of short strands of amino acids - peptides - and fatty acids, or lipids. One molecule works like glue, helping cells clump together into blobs, while the other acts more like string, letting them form chains. Together they give bacteria the ability to build communities - the sticky substance on your teeth - instead of floating alone.
The newfound gene cluster contains about 15 DNA segments coding for proteins, enhancers and transcription factors that act like a self-contained metabolic cassette - an alternative metabolic pathway that is not essential for survival of the bacteria but which, Zhang has found, has major impacts on the surrounding environment, such as teeth. These gene clusters are sometimes referred to as a microbe's secondary metabolism, but Zhang prefers the term "specialized" because they can produce interesting molecules. Specialized metabolic networks in soil bacteria have proved a fertile source of antibiotics, for example.
"These specialized metabolites enhance survival in certain ways," said Yao, one of three Berkeley graduate students who contributed to the work and are first authors of the paper. "Many, for example, are antibiotics, so they can kill other bugs, or others are involved in metal acquisition - they help the bacteria monopolize the resources in their environmental niche. Being able to produce these, especially in a microbial community, helps the bacteria boot out the other guy and guard their resources."
Yet the role of specialized metabolic networks and secondary metabolites in the human microbiome have largely remained unstudied, Zhang said. Two years ago, she and her colleagues found a gene cluster in oral bacteria that produces a previously unknown antibiotic. They found another gene cluster that produced a different set of sticky molecules that help to form biofilms.
Wenjun Zhang and McKenna Yao/UC Berkeley
The newly reported gene cluster is another demonstration of the importance of the microbiome's secondary metabolites in human health, whether in the mouth, gut, skin or any organ. Understanding these sticky metabolites in the mouth, dubbed mutanoclumpins, could help reduce cavities.
"We are looking for something which is correlated with cavities, with disease. If one day we can prove that, under certain conditions, this is really a bad molecule you want to prevent, we might develop genetic or chemical inhibitors to inhibit their production, so hopefully the bacteria will not make them, and you have fewer cavities," Zhang said. "Meanwhile, we also look at other molecules correlated with health, allowing a simple strategy to directly engineer the microbes to make more of them."
One species of bacteria that could use a boost is Streptococcus salivarius, which appears to promote oral health and is currently marketed as an oral probiotic. Unfortunately, even if it proves to be probiotic, it doesn't form a strong biofilm that sticks to teeth and rapidly dissipates. Zhang suggests adding strong biofilm-forming molecules to S. salivarius to see if the bacteria can work better as probiotics.
"Our future work will be to create a broad map of the collection of these specialized metabolites to look at collectively what this dynamic, complex community on your teeth is making," Zhang said.
Yao noted, however, that "the best way you can remove the biofilm on your teeth is to brush. We believe that there's actually a better way of disrupting that biofilm, but we're just beginning to understand what the complexity is within the mouth."
Nicholas Zill and Colin Charles Barber are first co-authors with Yao. Other co-authors are Yongle Du, Rui Zhai, Eunice Yoon and Dunya Al Marzooqi of Berkeley's Department of Chemical and Biomolecular Engineering and Peijun Lin, a visiting student in the College of Computing, Data Science, and Society.






