EMBL Barcelona researchers shed light on how the blood-brain barrier is damaged during severe malaria
Cerebral malaria is a severe complication of the disease that kills 1 out of 5 children that suffer from it, and causes long-term disabilities in half of the survivors. Malaria is caused by the parasite Plasmodium falciparum, which reproduces in our red blood cells and then breaks out of them to continue infecting new cells. Once the parasite makes it to the blood-brain barrier (BBB), a structure that protects the brain from harmful substances, it is able to damage it, causing severe complications.
Now, EMBL Barcelona researchers have created a lab-grown blood-brain barrier to show how the parasite damages it, and have successfully tested potential therapeutics that could help prevent or even reverse the damage. The work was published in the journal Nature Communications .
"You have to imagine the blood-brain barrier as a system of tightly sealed pipes that prevent leaks. The malaria parasite is capable of developing cracks in those pipes, and creating a leak that starts dripping infected fluid into the brain, causing swelling and making the disease irreversible," said Livia Piatti, Postdoctoral Fellow at EMBL Barcelona's Bernabeu Group and co-first author of the study.
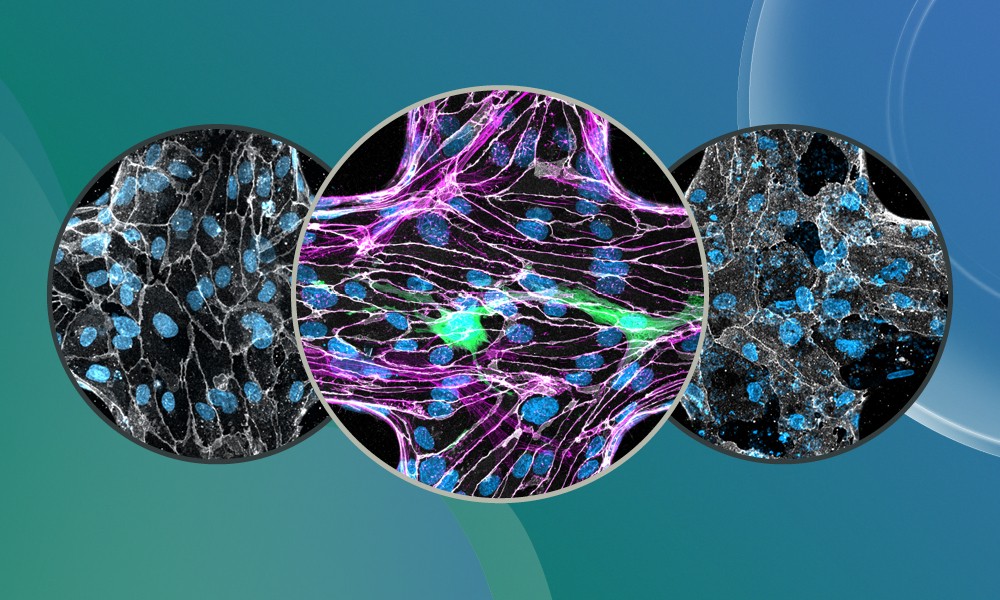
To understand how P. falciparum is able to damage the barrier, the Bernabeu Group built the most complete lab-grown infection model of the human blood-brain barrier to date. It includes the key cellular players: endothelial cells that line the blood vessels, supporting pericytes, and astrocytes, which are star-shaped brain cells, all arranged in a 3D structure with flowing fluid.
This miniature blood-brain-barrier-on-a-chip (3D-BBB) was then exposed to the parasite at its most explosive stage: the moment it bursts out of red blood cells in a process called egress.
"To assess barrier disruption, we used a live-imaging approach that tracked fluorescent molecules leaking from the inside of the vessels to the surrounding area. When we applied parasite egress products or infected red blood cells, we observed a significant increase in tracer passage, indicating that the barrier had become more permeable," said Alina Batzilla, Predoctoral Fellow in the Bernabeu Group and co-first author of the study.
In addition, analysis of gene expression at the single-cell level showed that cells were producing less of the proteins that keep the blood-brain barrier sealed, and more of the molecules that cause inflammation.
This study not only shows how and when the malaria parasite damages the blood-brain barrier, but it also points in the direction of treatment. The researchers successfully tested an approved drug, Ruxolitinib, on their 3D-BBB model, with results suggesting that it could be effective for deadly cases of malaria. Ruxolitinib is an inhibitor of the JAK-STAT signalling pathway, which activates an immune response, usually related to inflammation. In this study, blocking JAK-STAT signalling with Ruxolitinib acted as a patch to stop the dripping from the cracked pipes of the blood-brain barrier. By helping calm the inflammation in the blood vessels of the brain, the drug reduced the leakiness of the blood-brain barrier.
"Our 3D-BBB model is one of the most advanced to date, but we want to go further," said Maria Bernabeu, Group Leader and senior author of the study. "Our next step is to include immune cells and additional cell types present in the brain, like microglia and neurons. This will enhance the complexity of the model to make it as similar as possible to the real brain."






