Glioblastoma is the most common primary malignant brain tumour with a median overall survival within 1.5 years
Researchers from the School of Biomedical Engineering & Imaging Sciences have released a meta-analysis with findings suggesting there is poor evidence currently for studies using machine learning algorithms to determine if treatment of glioblastoma is effective.
The studies analysed by the researchers were deemed problematic as they appeared to be biased and researchers were also concerned as to whether those studies could be used in the clinic.
Our concerns related to flawed methods to determine the reference standard, ground truth, and how patients were selected in the studies. Many studies did not show whether the algorithms would work in hospitals outside of where the study was performed.– Dr Tom Booth, Reader in Neuroimaging, School of Biomedical Engineering & Imaging Sciences
Glioblastoma is the most common primary malignant brain tumour with a median overall survival within 1.5 years.
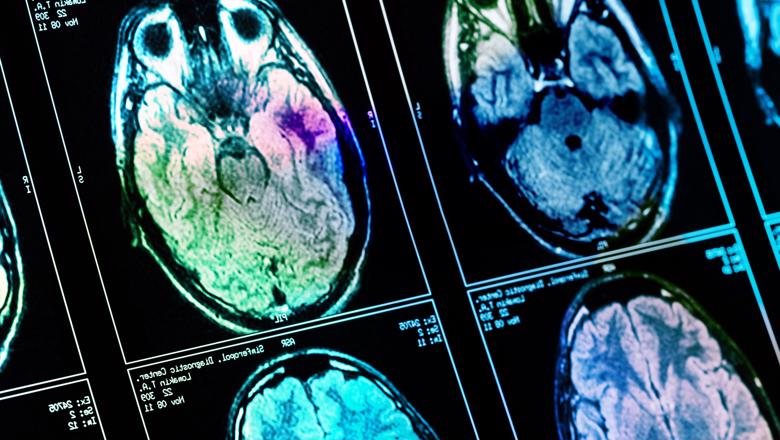
These brain tumours are followed up with magnetic resonance imaging (MRI) to see if there is a response to treatment.
If the treatment is working then it can continue. If not, second line treatment can be started. However, non-specific MRI appearances occur in approximately 50 percent of patients undergoing the standard treatment so it is often unclear if the treatment is working or not.
Many studies have used machine learning to overcome this lack of clarity so that treatment response can be determined accurately, which if comprehensively proven to work would be an important breakthrough.
The standard care regimen has been used since 2005 and consists of surgery, radiotherapy and a long course of chemotherapy. By 2008 it became apparent that doctors prescribing the regimen faced challenges from false-positive progressive disease which is known as 'pseudo-progression'.
This occurs during the 6-month period following the completion of radiotherapy and is manifest as an increase in contrast enhancement on MRI images, which reflects the non-specific disruption of the blood-brain barrier.
If there is true progression, the treating clinical team typically will initiate a prompt modification in treatment strategy with termination of ineffectual treatment or initiation of second-line surgery or therapies.
Alternatively, if there is pseudo-progression, the treating clinical team typically will continue with the standard care regimen.
However, the decision making can only be made retrospectively with current treatment response evaluation guidelines. A machine learning test applied to the MRI scan (i.e. a biomarker), that reliably distinguishes pseudo-progression from true progression at the time of increased contrast enhancement, would fully inform the difficult decision contemporaneously.
We have urged future researchers to use large, well-annotated datasets where there has been meticulous consideration regarding the ground truth. If this advice is taken up by the research community, the positive new developments in machine learning algorithms that are nearly ready for clinical adoption, will become enablers of better clinical care.– Dr Tom Booth, Reader in Neuroimaging, School of Biomedical Engineering & Imaging Sciences
The King's team are working hard to see action by leading a UK consortium to achieve these aims https://pubmed.ncbi.nlm.nih.gov/35616700/






