Using advanced imaging and minimally invasive techniques, UConn Health's lung cancer specialists guide patients through every step of their lung cancer journey.
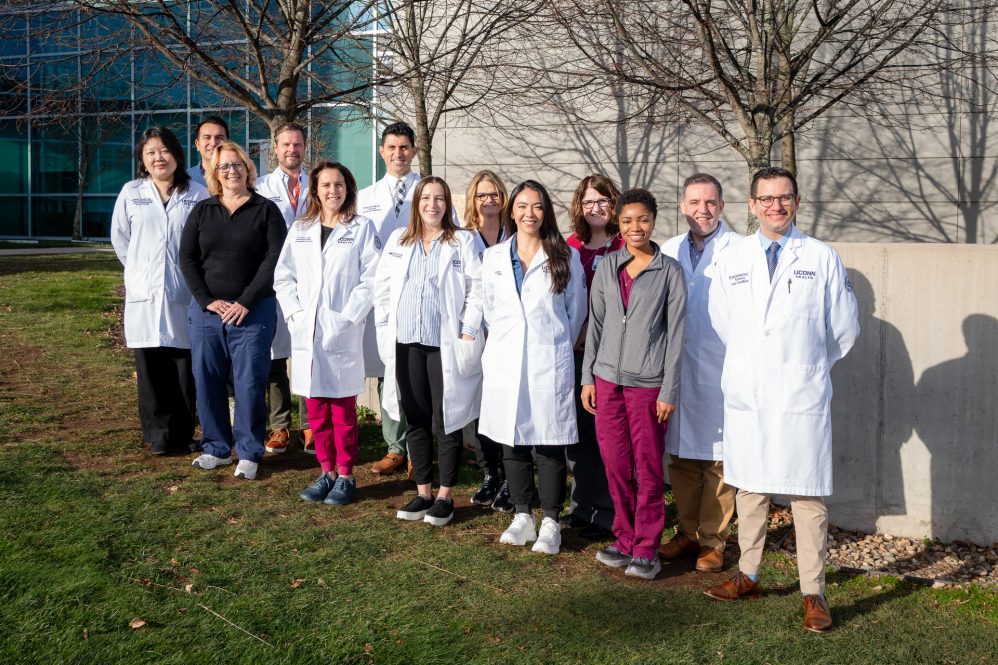
UConn Health Lung Cancer Team (Tina Encarnacion/UConn Health photo)
Lung cancer remains the leading cause of cancer deaths in the United States, making early detection, timely intervention, and multidisciplinary care critical. At UConn Health, a dedicated team of pulmonologists, radiologists, thoracic surgeons, oncologists, nurse navigators, and supportive specialists work together to provide coordinated, compassionate care for every patient-from initial screening through treatment and survivorship. Their goal is not only to fight cancer but also to support patients' overall health, breathing, and quality of life every step of the way.
Early Detection Saves Lives
The journey often begins with lung cancer screening, a cornerstone of UConn Health's approach to catching disease early. Cardiothoracic radiologists Dr. Electra Kaloudis and Dr. Jonathan Hargreaves lead the screening program, using low-dose CT scans that can detect lung nodules long before symptoms appear. These scans are far more sensitive than traditional chest X-rays and are especially effective in identifying cancers at a stage when intervention can be curative.
"Screening only works if patients come back every year," says Dr. Kaloudis. "Lung cancers often grow slowly, so regular, consistent imaging is the key to catching them early-before symptoms ever appear."
Screening coordinator Mark Taschereau plays a vital role in this process, reviewing each patient's history, verifying eligibility, and confirming follow-up schedules. He also updates smoking histories and answers patient questions to ensure everyone remains on track.
"This is not just a test," Kaloudis explains. "It's a program. People can easily drop off if no one is keeping track of their schedule. Continuity is essential."
Once scans are completed, radiologists use nationally established Lung-RADS guidelines to categorize findings and recommend next steps. For high-risk nodules, Dr. Kaloudis immediately coordinates with interventional pulmonology to plan minimally invasive biopsies or further evaluation.
UConn Health uses artificial intelligence (AI) to enhance its early lung cancer detection program, primarily through a software platform called the Virtual Nodule Clinic from the vendor Optellum. This AI technology is designed to identify potential lung nodules and help physicians diagnose patients at the earliest, most treatable stage possible.
Thanks to this structured, proactive approach, the majority of lung cancers detected at UConn Health are stage I or II-when treatment has the highest likelihood of success. Should a cancer be detected and treatment initiated, our cardiothoracic imaging team is there every step of the way to monitor effectiveness of therapy.
Pulmonology: Supporting Breathing Through Every Stage

Pulmonologists are central to the lung cancer care pathway, providing support that extends beyond diagnosis. Dr. Ethan Bernstein, a pulmonologist at UConn Health, plays a critical role in both identifying early disease and managing the pulmonary effects of cancer and its treatment.
"Patients often come to us for symptoms like shortness of breath, chronic cough, or COPD follow-up," Bernstein explains. "Sometimes, a routine scan reveals a small nodule, and that's how the cancer workup begins."
Pulmonology remains essential throughout treatment. Chemotherapy, radiation, surgery, and immunotherapy can all affect lung function, particularly in patients with pre-existing lung disease. Dr. Bernstein works closely with oncologists to manage side effects, such as inflammation or shortness of breath, ensuring patients can continue treatment safely and comfortably.
"Even if the cancer is responding beautifully, treatment itself can create complications," Bernstein says. "My job is to help people breathe better so they can keep fighting their cancer and living their lives."
Precision Diagnosis and Minimally Invasive Treatment

When a suspicious nodule is detected, interventional pulmonologist Dr. Omar Ibrahim, service chief of the UConn Health Carole and Ray Neag Comprehensive Cancer Center, often becomes the first physician to evaluate the patient. Using cutting-edge technology like the Monarch robotic bronchoscopy system, Ibrahim and his team can perform highly precise biopsies with real-time imaging and AI guidance. These techniques improve the speed and reliability of diagnosis while minimizing risk to patients.
"The technology allows us to navigate the lungs with incredible accuracy, getting a correct picture as quickly as possible," Ibrahim says. "It's safer, faster, and less stressful for patients than traditional methods and helps us plan the most effective treatment while minimizing unnecessary procedures."

Once a diagnosis is confirmed, the entire lung cancer team-including thoracic surgeon Dr. Dustin Walters-collaborates to develop a personalized treatment plan. Walters specializes in surgical management of diseases of the lungs, esophagus, and mediastinum. Using state-of-the-art minimally invasive and robotic-assisted surgical techniques, he performs procedures ranging from small wedge resections to full lobectomies, reducing pain and recovery time while maximizing treatment success.
"Every patient is different," Walters explains. "Our goal is to tailor surgery and treatment to their unique situation while integrating care from pulmonology, oncology, and radiation therapy."
Multidisciplinary Oncology Care
Medical oncologist Dr. Nathaniel Robinson and radiation oncologist Dr. Emily Lutz round out the core team. They design and deliver individualized treatment plans that may include chemotherapy, targeted therapy, immunotherapy, or precision radiation. For patients who cannot undergo surgery, stereotactic body radiation therapy (SBRT) provides a highly targeted approach that can sometimes be curative.

"Every patient's cancer is unique," Robinson says. "Our job is to match therapy to the biology of the tumor and the needs of the patient, balancing efficacy with quality of life."
Immunotherapy, which harnesses the immune system to attack cancer cells, has dramatically improved outcomes for many patients. Lutz notes, "Radiation therapy has become incredibly precise. We can target tumors to millimeter accuracy, sparing healthy tissue and reducing side effects. That precision makes a real difference in patient experience and outcomes."
Clinical trials provide additional options, allowing patients to access promising new therapies in Connecticut without traveling long distances. These studies may involve novel drugs, combination treatments, or innovative radiation techniques, offering hope to patients at every stage of disease.
Coordinated, Compassionate Care Every Step of the Way
At UConn Health, lung cancer care is never isolated. Nurse navigators, respiratory therapists, pathologists, and advanced practitioners ensure that every patient receives seamless, coordinated support. Tumor boards review each case, bringing together specialists to craft comprehensive care plans, while supportive services-nutrition, social work, pulmonary rehabilitation, and survivorship programs-address patients' physical, emotional, and practical needs.
"Our approach is about more than just treating cancer," Ibrahim emphasizes. "It's about guiding patients and families through a stressful time, giving them the information and support they need to make confident decisions."
From the first scan to the final treatment, UConn Health's lung cancer team combines innovation, expertise, and compassion, helping patients face lung cancer with hope and confidence. Every patient's journey is met with personalized care, advanced technology, and a collaborative network dedicated to improving outcomes, preserving quality of life, and offering renewed hope for the future.






