Key takeaways
- Internal organ tissues often don't heal after illness or injury and lose some function, such as the heart after a heart attack. UCLA cardiologists have identified a protein that interferes with healing.
- Funded entirely by federal and state grants, the researchers developed a drug to block this protein and promote tissue regeneration.
- The FDA has now granted approval to begin Phase I clinical trials of the first-in-class drug for tissue repair, called AD-NP1, in humans.
The body's tissues can get injured in many ways, but while some injuries heal perfectly, others don't heal at all. A cut in the skin, for example, usually heals all on its own, while internal organs, such as the heart after a heart attack or the kidney after an acute injury, remain damaged, leading to diminished function. Most tissues of the body repair themselves using the same processes, but until now, drugs that target these pathways to enhance tissue repair in slow-healing organs have not been identified. That's about to change.
UCLA cardiovascular scientist Arjun Deb discovered that heart tissue samples taken from mice and humans after a heart attack had increased levels of a protein called ENPP1. Deb and his scientific team observed that increased levels of ENPP1 initiated a metabolic chain of events that disrupted energy generation and function of multiple cells in the injured region of the organ, impeding tissue repair. The researchers found that blocking the production of ENPP1 enhanced heart repair and reduced the formation of scar tissue, thereby improving heart function.
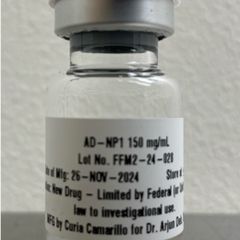
Backed entirely by funding from the National Institutes of Health, the Department of Defense, and the California Institute for Regenerative Medicine (CIRM), Deb's group developed a monoclonal antibody called AD-NP1 that shuts down the function of ENPP1 and promotes tissue repair in the heart and other organs. After experiments that showed its efficacy and safety in mice and monkeys, the FDA has now granted approval of the investigational new drug AD-NP1 for use in human clinical trials.
The achievement marks a rare instance of drug development going from bench to bedside in a single university laboratory, with no outside companies or investors involved. Often, drugs identified or engineered by academic researchers are licensed to private biotech companies for future development, or the scientist may spin off their own startup.
But Deb, who is a UCLA professor of medicine and molecular, cell and developmental biology and member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research, refused to take this route, persevering through seven years of research grants to develop a drug that has the potential to restore full function to hearts and other organs damaged by disease or injury.
"This work has been entirely funded by taxpayer dollars, and done entirely within the University of California research ecosystem," said Deb. "I have not taken a cent from any private donor or company to develop this drug. I hope this will form a model for future drug development at UCLA. This process has advantages of lower costs, potentially shorter development time and the principal investigator being in control of the science and having intellectual freedom with the development of the molecule, which is the most important of all."
Monoclonal antibodies are a class of drugs that are engineered in the laboratory and mimic the function of natural antibodies made by our immune system. Just like our immune system can produce specific antibodies to bind and inactivate specific pathogens, the monoclonal antibody, AD-NP1, has been specifically engineered to target human ENPP1 and no other human protein.
"Much like people eat food to get energy, cells also require energy to multiply and grow and function, and this is more critical when the tissue is injured," said Deb.
When biochemical pathways that generate energy within a cell are adversely affected, cellular function declines.
"That is what we saw: increased ENPP1 expression interfered with critical pathways that are needed for a cell to derive energy," said Deb, who added that when AD-NP1 was used in animals, the heart muscle had more energy and contracted much more vigorously, preventing the development of heart failure."
Because energy-generating pathways are the same between cell types, Deb and his team believe that AD-NP1 could benefit many other organs in addition to the heart after acute injury.
Deb's approach to tissue regeneration, which modulates metabolic pathways to foster tissue repair, is unique and does not involve the use of stem cells. "Rather, you use the power of the body's own repair system and optimize it to make it so much better," said Deb.
If clinical trials show that the drug works as well in humans as it does in animals, AD-NP1 could be first in a whole new class of tissue repair-enhancing drugs that prevent decline in organ function. Deb hopes his group can begin human trials soon.
"Cardiovascular disease is still the leading cause of death in the U.S. and around the world," said Deb. "All Americans want to lead healthier and longer disease-free lives. It's a testament to the funding system we have in place in this country that within six or seven years, in an academic lab in a university setting, we have engineered a new drug that potentially could be helpful to many people with heart disease or other forms of organ injury."






