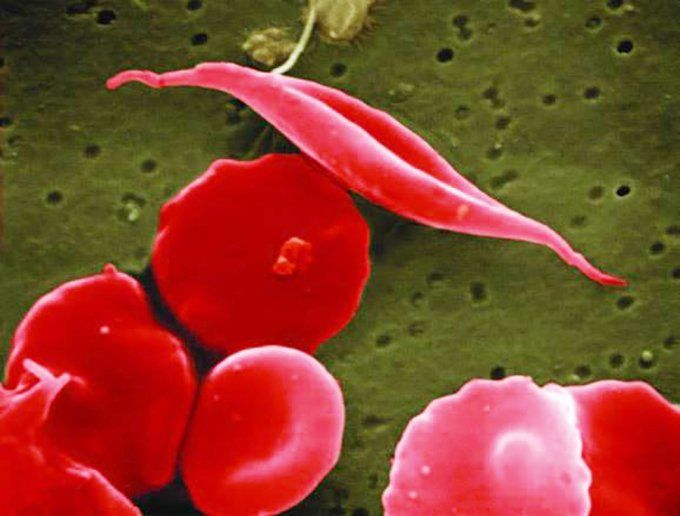
Sickle cell disease is a genetic blood disorder that affects the structure and function of hemoglobin, reduces the ability of red blood cells to transport oxygen efficiently, and progresses to a chronic vascular disease. Image by NIH
Scientists at UC San Francisco, UC Berkeley and UCLA have received U.S. Food and Drug Administration approval to jointly launch an early phase, first-in-human clinical trial of a CRISPR gene correction therapy in patients with sickle cell disease using the patient's own blood-forming stem cells.
The trial will combine CRISPR technology developed at Innovative Genomics Institute (IGI) - a joint UC Berkeley-UCSF initiative founded by Berkeley's Nobel Prize-winning scientist Jennifer Doudna, PhD - with UCLA's expertise in genetic analysis and cell manufacturing, and the decades-long expertise at UCSF Benioff Children's Hospital Oakland in cord blood and marrow transplantation and in gene therapy for sickle cell disease. The 4-year study will include six adults and three adolescents with severe sickle cell disease. It is planned to begin this summer in Oakland and Los Angeles.
The trial aims to directly correct the sickle mutation in blood stem cells that causes them to create deformed red blood cells, leading to the debilitating and painful disease, according to Mark Walters, MD, a professor of pediatrics at UCSF and principal investigator of the clinical trial and gene editing project. It will be the first time clinical researchers attempt to correct the faulty beta-globin gene in a patient's own cells with non-virally delivered CRISPR gene correction tools. Previously, researchers have used more costly and indirect approaches such as reactivating fetal hemoglobin or using viral vectors to suppress the gene that turns off the fetal globin production at birth.

Mark Walters, MD, is a principal investigator of the clinical trial and gene editing project. Photo by Barbara Ries
"This therapy has the potential to transform sickle cell disease care by producing an accessible, curative treatment that is safer than the current therapy of stem cell transplant from a healthy bone marrow donor," said Walters, who is also the Jordan Family Director of the Blood and Marrow Transplant Program at UCSF Benioff Children's Hospital Oakland. "If this is successfully applied in young patients, it has the potential to prevent irreversible complications of the disease."
Sickle cell disease is a genetic blood disorder that affects the structure and function of hemoglobin, reduces the ability of red blood cells to transport oxygen efficiently, and progresses to a chronic vascular disease that affects approximately 100,000 Americans and millions worldwide, with a disproportionate effect on the Black community.
The disease is caused by a single-letter change, or mutation, in human DNA. This trial will use CRISPR genome editing to correct this mutation directly. The project team from UCSF, the IGI, and UCLA have developed CRISPR_SCD001, a patient-specific blood stem cell therapy that has been modified by a CRISPR-Cas9 nuclease to stimulate repair of the sickle mutation. In this approach, the patient's blood stem cells will be extracted and sent to UCLA's gene manufacturing lab to undergo a process known as electroporation, in which cells are exposed to electrical pulses that create temporary pores in their membranes. These pores allow the CRISPR-Cas9 platform to enter the blood stem cells and travel to the cells' nuclei, where it corrects the sickle cell mutation before the cells are reintroduced to the patient.






